Researchers Identify Gene Mutations Likely Promoting Pituitary Tumor Growth in Cushing’s Disease
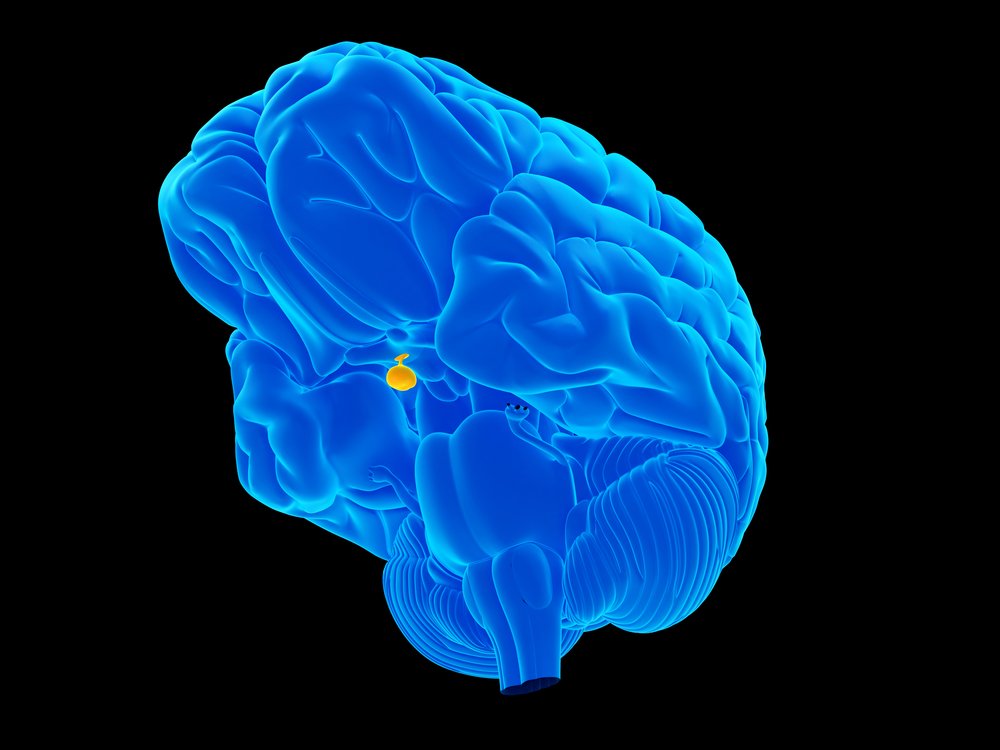
Mutations in a gene called CABLES1 might contribute to pituitary tumor growth in people with Cushing’s disease, according to a study that suggests the gene normally acts as a pituitary tumor suppressor.
The study, “Loss-of-function mutations in the CABLES1 gene are a novel cause of Cushing’s disease,” published in the journal Endocrine-Related Cancer, also showed that CABLES1 affects molecular pathways that link genes, previously associated with Cushing’s disease development.
Researchers at the Eunice Kennedy Shriver National Institute of Child Health and Human Development figured out that the gene might be involved in the propensity to grow pituitary tumors in people with Cushing’s.
While Cushing’s can also be caused by glucocorticoid drugs, the vast majority of patients develop Cushing’s disease because of cortisol-producing tumors.
Their guess was not random. Researchers know that the CABLES1 gene acts to suppress cell division in certain pituitary cells in response to cortisol. Therefore, they turned to an observational study of pituitary tumors (NCT00001595) and identified 146 children and 35 adults with Cushing’s disease.
Analyzing DNA in blood or tumor samples, researchers found four so-called missense mutations in CABLES1, in which a change in a single DNA base causes a change in amino acid in the resulting protein. These mutations, found in the normal, non-cancerous DNA of two children and two young adults, made a CABLES1 protein that was unresponsive to cortisol.
In three of the patients, researchers could not establish whether patients had inherited mutations from their parents or if they had appeared spontaneously.
These patients had large tumors requiring repeat surgery — in one case complemented with radiotherapy.
Experiments in lab-grown pituitary tumor cells revealed that the four mutations led to a lost ability to suppress cell growth in response to cortisol.
“The mutations we identified impair the tumor suppressor function in the pituitary gland,” Constantine A. Stratakis, MD, the study’s senior study, said in a press release.
“This discovery could lead to the development of treatment strategies that simulate the function of the CABLES1 protein and prevent recurrence of pituitary tumors in people with Cushing syndrome,” added Stratakis, who is also director of the NICHD Division of Intramural Research.
It is not the first time CABLES1 has been linked to tumor growth. Earlier studies have shown that the CABLES1 protein is lost in endometrial, ovarian, colorectal, lung, and squamous cell carcinomas.
The team also noted that their findings could link two other observations in patients with corticotropin-producing pituitary tumors. Such patients have an overactive EGFR (epidermal growth factor receptor) molecular pathway and a lower activity in a so-called CDK/cyclin-dependent pathway that controls cell divisions.
The increased activity in EGFR can inactivate CABLES1, which normally acts to control CDK/cyclin.






