New ACTH Detection Method Improves Cure Rates in Cushing’s Disease Patients, Study Shows
Researchers have identified a new, quick method for detecting ACTH-producting tumors – called Elecsys – that can improve the cure rates of Cushing’s disease patients undergoing surgery.
The study, “Long-term outcomes of tissue-based ACTH-antibody assay–guided transsphenoidal resection of pituitary adenomas in Cushing disease,” was published in the Journal of Neurosurgery.
Transsphenoidal resection (TSR) – a surgical procedure performed through the nose and sphenoid sinus to remove a pituitary tumor – has been the method of choice for treatment for Cushing’s disease.
However, it often fails to localize the tumor with precision, leading to an incomplete resection (removal). This is likely a result of the preoperative methods used to guide surgeons before surgery, which include both magnetic resonance imaging (MRI) and a minimally invasive procedure called bilateral inferior petrosal sinus sampling (BIPSS) that measures ACTH in the veins that drain the pituitary gland.
However, both “suffer from suboptimal sensitivity and thus allow for incomplete resections, specially if pathological frozen sections fail to identify tumor,” researchers wrote.
MRI, for example, detects only 50 percent of Cushing’s adenomas, limiting surgeons’ ability to conduct curative TSR surgeries. Therefore, better diagnostic and tumor localization techniques are needed to increase the likelihood that initial surgeries can remove the entire tumor and cure patients.
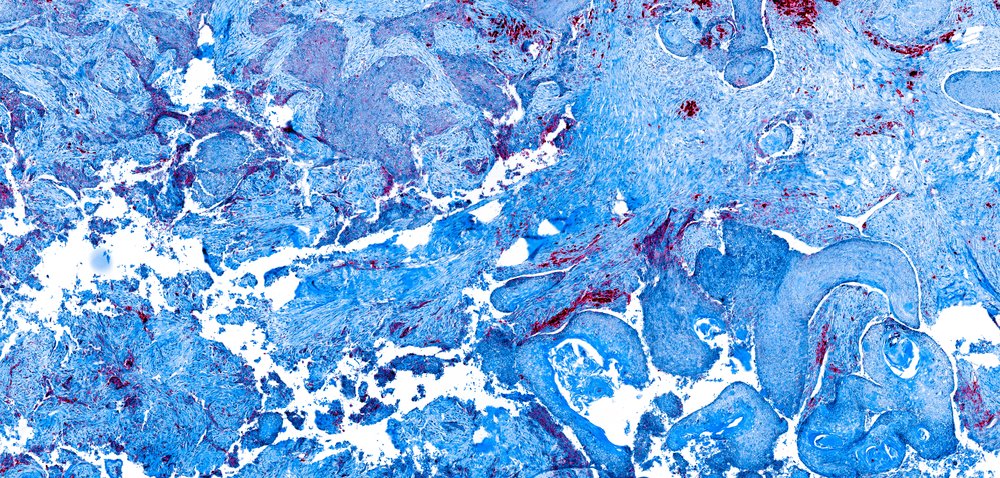
A team of researchers at Yale School of Medicine evaluated a new method for guiding tumor localization during TSR. The method – a double-antibody sandwich assay for ACTH – is performed in the operating room in resected pituitary samples from patients. ACTH (adrenocorticotropic hormone) is a hormone produced in the pituitary gland in the brain, that simulated cortisol production in the adrenal glands. In patients with Cushing disease the pituitary gland releases too much ACTH.
In the new method – called Elecsys – samples are squeezed between sandwich-like system composed of two antibodies that recognize two sections of the ACTH protein. The three-step procedure is quick, allowing doctors to analyze samples in the operating room and determine if they have removed the entire tumors.
The performance and outcomes associated with the Elecsys were assessed by reviewing data of tissue samples from 14 patients with ACTH-secreting adenomas, who underwent TSR surgeries between 2009 and 2014.
“The intraoperative TSR protocol was modified with the introduction of the ACTH assay such that if either the assay or the frozen-section pathology returned results positive for tumor, that area of the gland was resected,” the researchers explained.
The new ACTH method detected tumor tissue and was capable of distinguishing it from normal tissue with a 95% sensitivity and 71.3% specificity. These values are comparable to those using the standard method for tumor localization, which requires frozen sections of the tumor. This suggests that the test can be used either in conjunction with or in place of frozen sections.
Also, 85.7% of the patients achieved long-term disease remission, with the remission rate exceeding the rate with previous methods (71.9%).
Overall, “these preliminary findings reflect the promising potential of tissue-based ACTH-antibody-guided assay for improving the cure rates of Cushing’s disease patients undergoing TSR. Further studies with larger sample sizes, further refinements of assay interpretation, and longer-term follow-ups are needed,” the study concluded.






