CyberKnife Radiosurgery Effective in Cushing’s Disease, Research Finds
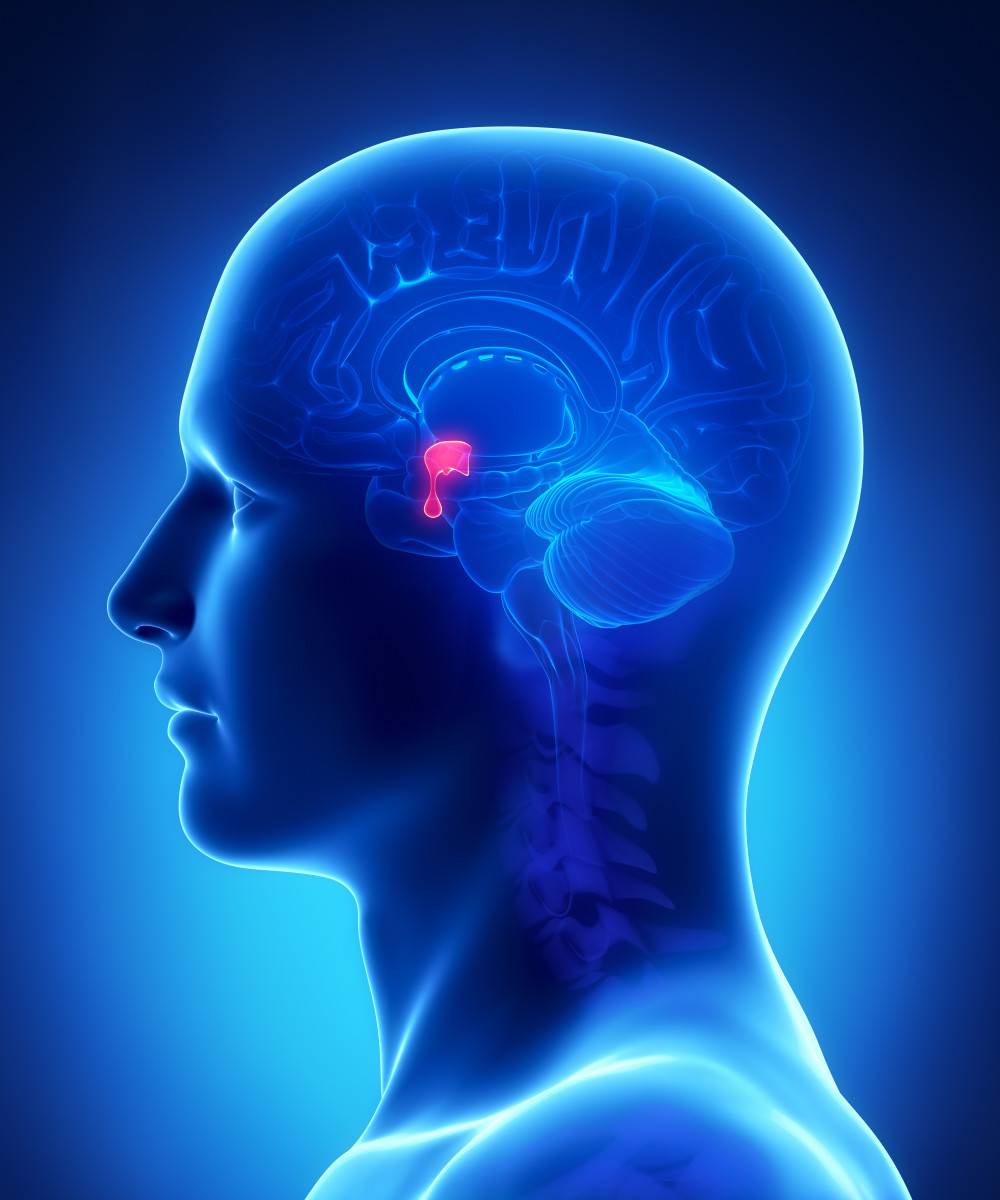
CLIPAREA l Custom media/Shutterstock
Stereotactic radiosurgery – a type of targeted, high-dose radiation therapy – delivered with CyberKnife technology effectively induces remission in Cushing’s disease patients whose condition persisted after surgical removal of their pituitary glands.
However, researchers advise, caution when interpreting the findings. While promising, the study included only a small group of patients analyzed retrospectively.
The study, titled “CyberKnife Radiosurgery in the Multimodal Management of Patients with Cushing’s Disease,” was published in the journal World Neurosurgery.
Stereotactic radiosurgery (also known as CyberKnife or Gamma Knife surgery, depending on the machine that is used) is a non-invasive procedure that involves exposing a very small area to high doses of radiation. It often is used to destroy small brain tumors and pituitary tumors. (The pituitary gland is located at the base of the brain.)
Cushing’s disease usually is due to a pituitary tumor that produces excess adrenocorticotropic hormone (ACTH), a hormone that causes cortisol levels in the blood to rise.
To date, no studies have assessed the outcomes of Cushing’s patients treated with CyberKnife technology. So, researchers at Stanford University decided to investigate if stereotactic radiosurgery could be useful at normalizing cortisol levels in patients where surgery had not been successful.
The study examined the medical records of seven patients with Cushing’s disease who had undergone transsphenoidal surgery to remove pituitary tumors, and whose disease had either persisted or recurred afterward.
Transsphenoidal surgery is a procedure to remove pituitary tumors. It is performed through a hollow space in the skull behind the nasal passages and below the brain. No part of the brain is touched during the surgery, so the possibility of damaging the brain is very low.
In this study, CyberKnife radiosurgery was done following the transsphenoidal surgery after a period of time that ranged around 14 months. Patients’ disease status was assessed after an average of 54.4 months of follow-up.
Normalization of blood cortisol levels was achieved in four patients, or 57.1 percent. Among them, two achieved normalization of the hypothalamic pituitary adrenal (HPA) axis without the need for hormone replacement. The HPA axis is a network in the body that regulates stress responses and cortisol levels.
The other two, developed hypoadrenalism – characterized by low levels of adrenal hormones – and required hormone replacement therapy. The time from radiosurgery to remission was about 12.5 months.
Researchers concluded that CyberKnife radiosurgery improved Cushing’s disease in this small sample of patients. They noted that the patients who underwent CyberKnife radiosurgery less than 14 months after transsphenoidal surgery had significantly better outcomes.
“In a small number of patients with CD, we demonstrate that CK is an effective treatment, with rare complications,” the investigators concluded.






