Study Highlights Importance of Clinical Follow-Up in Cushing’s Patients After Adenoma Removal
Written by |
A rare case of Cushing’s syndrome (CS) in a 17-year-old patient with multiple pituitary adenomas highlights the importance of clinical follow-up in order to determine the best treatment options for patients.
The study, “A rare case of multiple pituitary adenomas in an adolescent Cushing disease presenting as a vertebral compression fracture,” was published in the journal Annals of Pediatric Endocrinology and Metabolism.
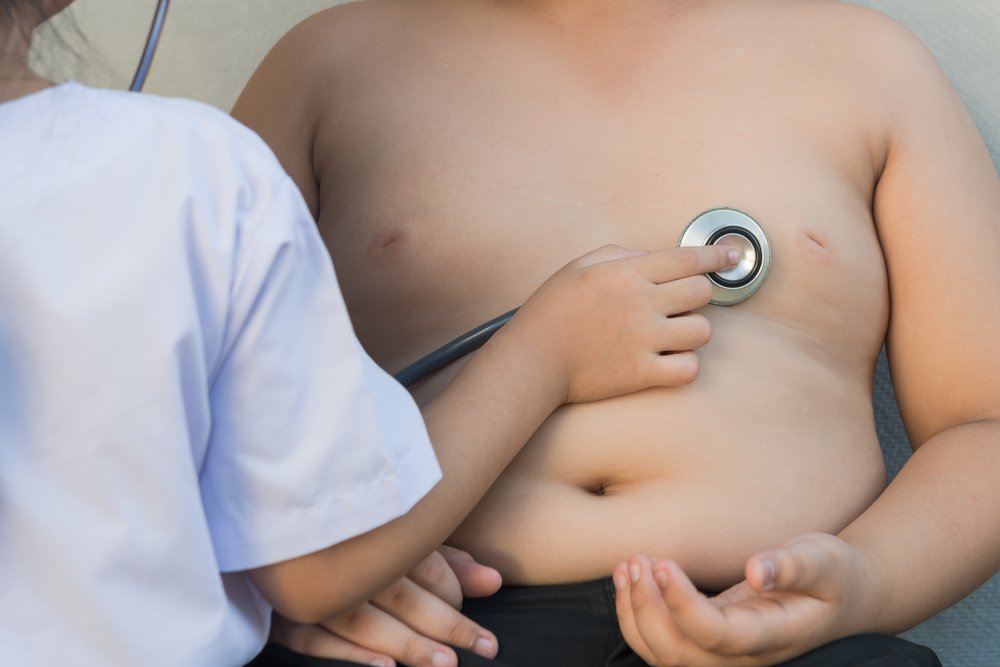
CS is a very rare disease with an incidence of 0.7-2.4 cases per million, per year. It is caused by exposure to very high levels of the hormone cortisol. In children, the most common symptom is weight gain without height gain. In some rare cases, tumors known as multiple pituitary adenomas (MPAs) appear, and patients have elevated levels of adrenocorticotropic hormone (ACTH). Surgical removal through transsphenoidal surgery (TSS) is considered the best treatment, and the first TSS has a success rate of more than 90%.
However, since 15% of patients have a recurrence, ongoing monitoring and follow-up after TSS are important. The importance of this follow-up care is highlighted in a recent case report.
The study described the case of a 17-year-old male adolescent who was 149.5 cm tall (4’9″) and weighed 63.6 kg (140 lbs). The patient was referred to a hospital for the evaluation of a vertebral compression fracture and obesity. Over four years, the patient gained 23 kg (51 lbs) without an increase in height. Despite showing many of the features of CS, this patient had not been previously diagnosed with CS.
He had high levels of ACTH and cortisol, and an MRI suggested the presence of an 8-mm (0.8 cm) micro-adenoma. After TSS, the patient’s morning ACTH and cortisol levels were reduced, and a persistent headache had improved. But there was no reduction in weight.
Three months after the TSS, the patient’s body mass index did not show improvement, and both cortisol and ACTH levels were elevated again. MRI revealed a new 9 mm (0.9 cm) micro-adenoma, which was removed with a second TSS. However, cortisol and ACHT remained elevated after the second surgery, with no evidence of a pituitary tumor in MRI scans.
Researchers recommended additional options, such as total removal of the pituitary gland, radiotherapy, or removal of both adrenal glands, options that the patient and his family declined. He continued to receive treatment for osteoporosis, hypertension, and increased lipid levels.
“In conclusion, we reported the clinical course of Cushing disease with 2 distinct pituitary adenomas. Since there is no consensus as to the best treatment for relapsing or persistent Cushing disease and since only a few cases of MPA among pediatric Cushing disease have been reported, a close followup of tumor status, severity of hypercortisolism, and patients’ perspectives are the major parameters used to determine the best treatment option for each patient. In addition, early recognition and diagnosis of pediatric Cushing disease would lead to earlier recovery, improved growth, and better quality of life,” the researchers wrote.





