FAQs about Cushing’s disease diagnosis
Diagnosing Cushing’s disease involves multiple tests that are used to measure the levels of adrenocorticotropic hormone (ACTH) and cortisol in the body, as well as to look for a tumor in the brain’s pituitary gland. The disease is caused by a pituitary tumor that secretes ACTH, which drives the excess production of cortisol that ultimately gives rise to Cushing’s disease symptoms.
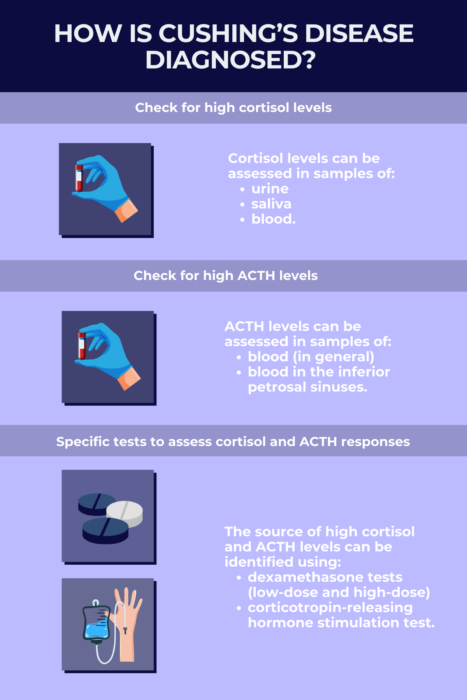
Tests to diagnose Cushing’s disease, which can include a test of the urine, blood, or saliva, seek to determine if there is a tumor in the body’s pituitary gland. Such tumors can cause Cushing’s disease by triggering the production of high levels of cortisol in the body by secreting a signaling molecule called adrenocorticotropic hormone (ACTH). Among the tests to diagnose the cause of Cushing’s are measurements of cortisol and ACTH levels in blood and/or urine samples, as well as diagnostic procedures like the dexamethasone suppression test or corticotropin-releasing hormone (CRH) stimulation test, which can assess imbalances in cortisol and ACTH production.
Cushing’s disease is characterized by high levels of two hormones: adrenocorticotropic hormone (ACTH) and cortisol. Measuring levels of these hormones in blood or other bodily fluids is usually a key first step in establishing a diagnosis of the disease.
Imaging tests like MRI and CT scans can be helpful for visualizing tumors in the pituitary gland, but not all such growths are disease-causing. Cushing’s disease is caused by a tumor in the pituitary that secretes high levels of adrenocorticotropic hormone (ACTH), so visualizing the tumor can help to confirm the diagnosis and guide decisions about surgery or other treatments. However, many people have benign growths in the pituitary gland that don’t cause overt health problems, so imaging alone is not sufficient to diagnose Cushing’s disease — additional tests to detect hormone changes are needed.
Multiple different tests may be used to help confirm a diagnosis of Cushing’s disease. While any of these tests individually has some risk of false results, many common assessment measures — like petrosal sinus sampling, dexamethasone suppression tests, and corticotropin-releasing hormone (CRH) stimulation tests — are typically more than 90% accurate for detecting the disease. By combining these different tests, clinicians can diagnose the disease with a very high level of accuracy.
Related Articles

 Fact-checked by
Fact-checked by