Circadian Rhythm Changes Seen to Link Hormonal Disorders and Obesity in Animal Study
Written by |
Obesity can be triggered by detrimental changes to the normal daily rhythms of hormone production, leading to an increased production of fat cells, research in mice shows.
These findings help to explain why conditions that disturb hormone levels, such as Cushing’s disease and stress, raise a person’s risk of obesity.
The study, “A Transcriptional Circuit Filters Oscillating Circadian Hormonal Inputs to Regulate Fat Cell Differentiation” published in the journal Cell Metabolism, analyzed how abnormalities in the daily oscillations, or rhythm, of glucocorticoid hormone levels lead to an excess accumulation of body fat.
Glucocorticoids are a class of hormones important to maintaining a balance in the workings of the immune system, and sugar and fat metabolism.
Problems in glucocorticoid action has been linked to severe metabolic diseases, including obesity, insulin resistance, and type 2 diabetes.
Glucocorticoids can trigger the production of fat cells, called adipocytes, that primarily compose fat tissue. How these hormones control fat cell production, however, is not fully understood.
Cortisol is the major glucocorticoid hormone in people, and key to controlling blood-sugar levels and inducing the breakdown of fats and proteins. It is also an important hormone in stress signaling.
In mammals, glucocorticoids have a daily oscillation that follows our 24-hour internal clock, called the circadian rhythm. The level of these hormones peak in the morning, drop during the day, and reach their lowest values at night.
It is known that people with abnormal levels of glucocorticoids, such as Cushing’s patients — whose levels of cortisol are higher-than-usual and more flat than oscillating — are prone to obesity.
Chronic stress, irregular eating or sleep cycles, and prolonged treatment with glucocorticoid drugs, including dexamethasone and hydrocortisone, are also known to disturb glucocorticoid levels and correlate with obesity.
Researchers suspected that human cells have a system to sense the daily rhythm of glucocorticoids, keeping the production of fat cells low in healthy individuals (only 8% of fat cells renew each year). When that hormone rhythm is disrupted, the system’s response turns awry and fat cells production rises.
Their investigation looked into the mechanism behind such fat cell production.
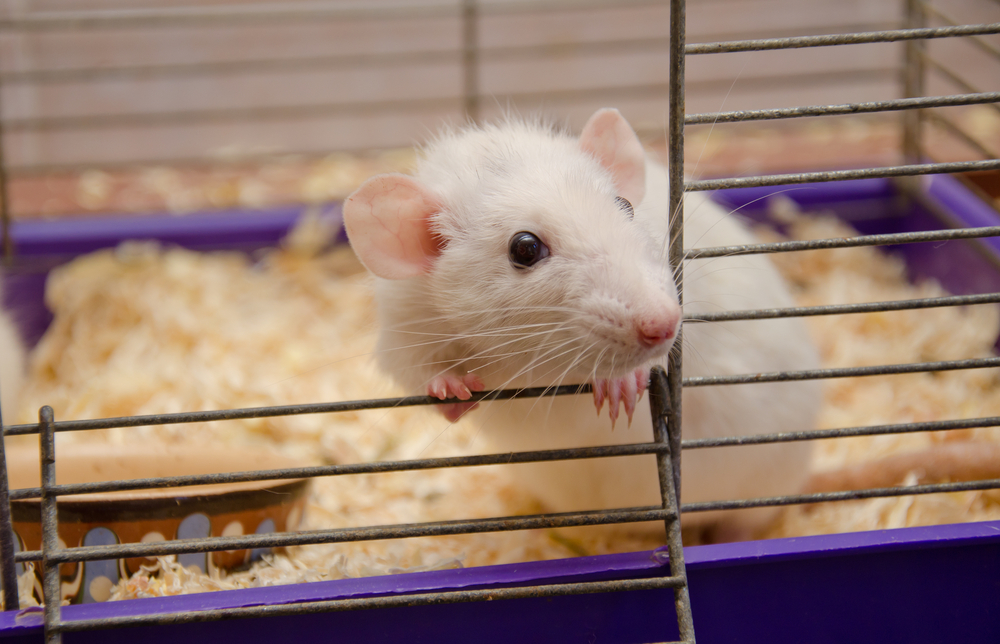
To do this, the researchers engineered mouse preadipocytes (precursors of fat cells) to produce fluorescent proteins linked with two key regulators of fat cell production, called PPARG and CEBPB.
By measuring the fluorescent signals, they could track the levels of PPARG and CEBPB and the transformation of preadipocytes into fat cells.
Treating those cells with rhythmic or continuous hormone doses, they could also measure the effect of each hormone regimen in the differentiation of fat cells.
Data showed that rhythmic cycles mimicking daily hormonal variations are “rejected” by preadipocytes, resulting in minimal differentiation of fat cells.
But increasing numbers of fat cells start to be produced when the hormone pulses extend beyond normal and stay constant for more than 12 hours.
Detailed analysis of PPARG and CEBPB indicates that both factors are rapidly destroyed when hormone levels are oscillating, keeping them below the threshold level for fat cell differentiation.
But when glucocorticoid hormones are constant, a signaling circuit that amplifies PPARG ends up triggering fat cell differentiation.
Importantly, researchers tested if oscillating versus continuous levels of corticosterone, the major glucocorticoid hormone of rodents, affected how fat mass accumulates in mice.
They did. Body weight and fat mass increased significantly in mice with constant levels of the hormone, compared to those with a normal circadian oscillation.
Overall, these findings help to explain the molecular mechanism behind an increased risk of obesity and diseases liked to disturbed hormone production. They could help in developing new treatments, or in adapting existing ones to better adjust hormone levels changes throughout the circadian rhythm.
“Together, our study provides a molecular mechanism for why stress, Cushing’s disease, and other conditions for which glucocorticoid secretion loses its pulsatility may lead to obesity,” the researchers wrote.
“[T]he molecular filtering mechanism for differentiation we uncovered for adipocytes provides support for the development of temporal therapeutic regimens aimed at changing adipogenic or other hormone pulse durations to control differentiation of precursor cells,” they concluded.