Repeat Stereotactic Radiosurgery Linked to High Remission Rates, Study Finds
Written by |
Repeat radiation therapy may be a reasonable third-line option for patients with persistent Cushing’s disease, after pituitary surgery and initial radiation therapy, a new study shows.
Durable remission was seen in 50 percent of patients who received the treatment, according to the study.
The research, titled, “Repeat stereotactic radiosurgery for Cushing’s disease: outcomes of an international, multicenter study,” was published in the Journal of Neuro-Oncology.
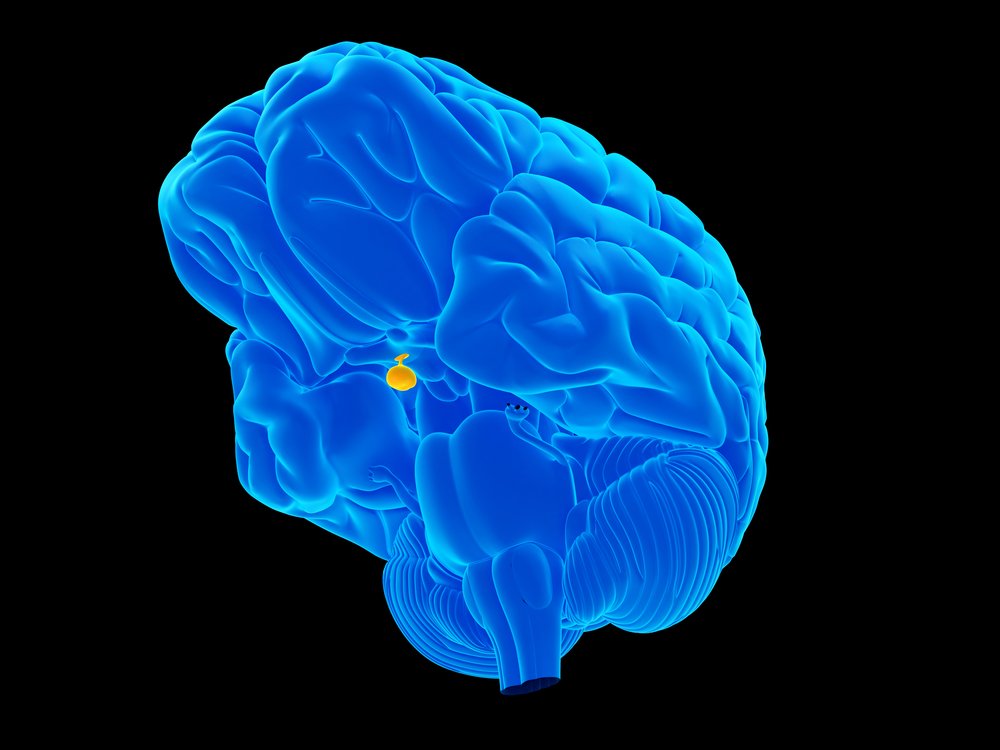
Cushing’s disease is characterized by the presence of masses in the pituitary glands that produce an excess of adrenocorticotropic hormone (ACTH), leading to high cortisol levels.
The primary treatment for Cushing’s disease is pituitary surgery, which induced remission in 65-90 percent of patients. For patients whose pituitary surgery was unsuccessful, a number of strategies may be offered, including stereotactic radiosurgery (SRS).
SRS is a type of radiation therapy that uses several precise radiation beams to target tumors. The method uses 3D imaging to detect the affected region and minimize the impact on surrounding healthy tissues.
A recent study reported durable endocrine remission in 64 percent of Cushing’s disease patients 10 years after receiving second-line SRS. But the benefit of repeating SRS in patients who do not achieve or maintain remission after SRS has not been reported.
Researchers at the University of Virginia Medical Center aimed to investigate the results of repeat SRS in patients who did not respond to prior surgery and SRS.
The study involved 20 CD patients who had been treated with repeat SRS with six or more months of follow-up. The median time from initial SRS to repeat SRS was three years. The median prescription dose was 20 Gy (the units of absorbed radiation dose), which was lower than the 25 Gy used in the initial SRS.
Endocrine remission occurred after a median of six months in 12 patients (60%). But two of these patients experienced biochemical recurrence, or high cortisol levels. Ten of these patients (50%) achieved durable endocrine remission.
Despite repeat SRS, 10 patients experienced persistent hypercortisolism. Three of these patients did not achieve remission despite a third repeat of SRS.
Of the 20 patients, two experienced adverse radiation effects after repeat SRS. This is considered similar to what is observed in SRS for pituitary tumors in general.
One advantage of SRS is that although the observed remission rates are similar to those that can be obtained by other medical options, such as ketoconazole and metyrapone, SRS does not require lifelong therapy.
“These data suggest that repeat SRS is an additional therapeutic option for patients with persistent CD despite pituitary surgery and initial SRS,” the researchers stated. Furthermore, “the possibility of permanent cure and freedom from lifelong medical therapy makes this an attractive option for appropriately selected patients, particularly those who are resistant to or cannot tolerate medical therapy.”





