Stronger MRI Enables Precise Spotting of Tumor Location in Cushing’s Disease Patients, Case Report Shows
Written by |
Using magnetic resonance imaging (MRI) with superior magnetic strength enabled determination of precise tumor location in a patient with Cushing’s disease, a new case report describes.
The research, “Value of pituitary gland MRI at 7 T in Cushing’s disease and relationship to inferior petrosal sinus sampling: case report,” appeared in the Journal of Neurosurgery.
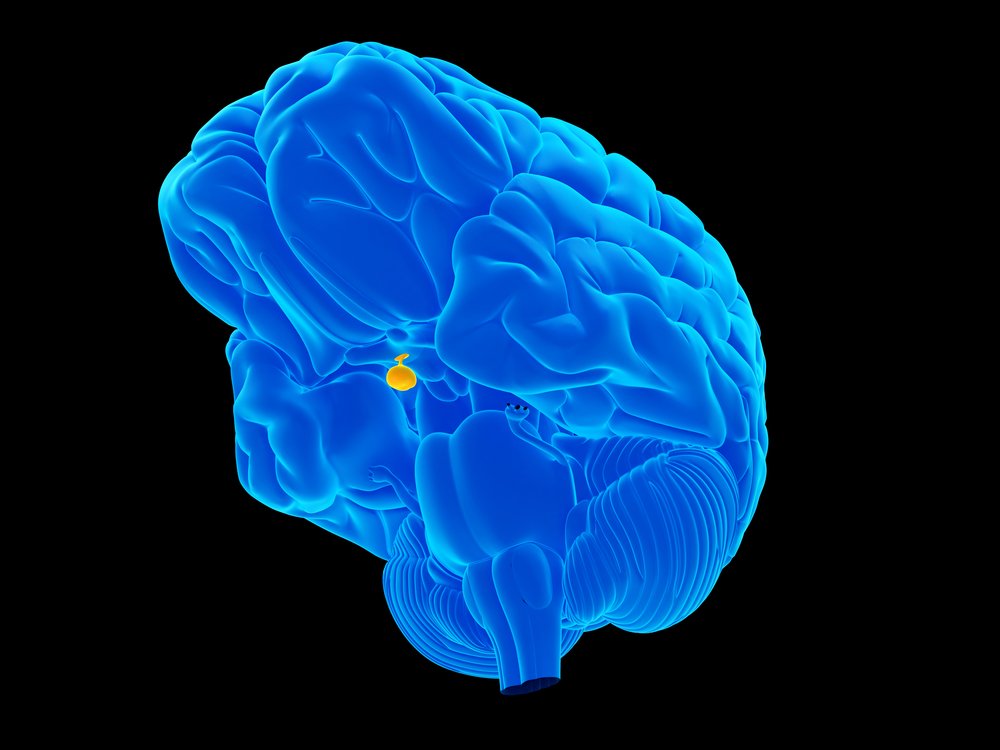
Cushing’s disease is the most common form of Cushing’s syndrome. It is caused by a pituitary adenoma (a tumor arising from the pituitary gland, located at the base of the brain) producing excessive levels of adrenocorticotrophic hormone (ACTH), which then lead to overproduction of cortisol in the adrenal gland.
Most Cushing’s adenomas, called corticotroph adenomas, are smaller than 10 mm in diameter (microadenomas), which complicates diagnosis with MRI. These limitations require using the gold standard of inferior petrosal sinus sampling (IPSS) coupled with MRI for final diagnosis. IPSS samples ACTH levels directly from the veins that drain the pituitary gland. But in addition to being an invasive method, it also is a poor predictor of tumor location.
MRI at 1.5 Tesla (T) — the unit of measurement of the magnet strength — is commonly used in Cushing’s disease patients, but research showed that 36-63% of pituitary microadenomas remain undetected. MRI at 3-T demonstrated superior sensitivity and researchers hypothesize that 7-T may lead to even better results.
The scientists presented the case of a 27-year old woman with a history of amenorrhea, which refers to absence of menstruation. Upon stopping taking oral contraceptives, the patient gained weight and lost hair, which was associated with coarsening hair on the face, while also having easy skin bruising, insomnia, and anxiety.
Although physical examinations revealed she was generally healthy, laboratory results showed elevated urinary free cortisol excretion and midnight salivary cortisol. The patient also had high levels of the steroid hormone DHEA, but normal amounts of ACTH.
Use of a 1.5-T MRI did not detect microadenoma. Bilateral IPSS revealed a central to peripheral and a right to left gradient, as the baseline ACTH level was 560 pg/ml on the right (well above normal) and 15 pg/ml on the left. This indicated that the source of the ACTH secretion was at the center right of the pituitary.
These findings led to the recommendation of surgery to remove the presumed pituitary microadenoma. Two hours prior to surgery, the patient underwent 3-T and 7-T MRIs.
Similar to 1.5-T, 3-T MRI revealed what appeared to be a normal pituitary gland. However, the higher resolution of the 7-T MRI revealed a potential 8 mm right-sided microadenoma, which correlated with the IPSS results.
“This 7-T MRI study provided additional support regarding tumor location for the neurosurgeon to proceed to surgery,” the scientists wrote.
The removed tumor was then analyzed, which confirmed the excessive production of ACTH and prolonged hypercortisolemia, which means abnormally high amounts of circulating cortisol.
The patient’s ACTH levels were greatly reduced within three days post-surgery, which ultimately led to nausea, fatigue, and headache. She was then prescribed 20 mg hydrocortisone twice a day to treat adrenal insufficiency from the surgery and discharged home.
The patient subsequently showed improvements in skin bruising and in fat loss/distribution, as well as normalized hormonal levels and menstrual function, even after discontinuation of glucocorticoid hormone replacement.
“Pituitary MRI at 7-T presented clearer visualization of a pituitary microadenoma in a patient with confirmed Cushing’s disease than 1.5-T and 3-T MRI did,” the investigators wrote.
“In the future, 7-T MRI may become more routine and possibly preempt IPSS in patients who have Cushing’s disease that is considered MRI negative based on standard 1.5-T and 3-T imaging studies,” they added.





