New Therapeutic Target Found to Suppress Pituitary Tumors
Researchers analyzed the gene activity of individual cells in adenomas
Written by |
Single-cell analysis of non-cancerous pituitary gland tumors that cause Cushing’s disease identified a novel therapeutic target with the potential to suppress tumor cell growth, a study has revealed.
Although cells from such tumors, called adenomas, had excess production of noxa — a protein that stimulates cell death — noxa was quickly degraded.
Blocking noxa degradation with an approved cancer medication, at therapeutically relevant doses, suppressed the growth of adenoma cell lines derived from multiple Cushing’s patients, demonstrating this target’s therapeutic potential, the researchers said.
The study, “Pituitary adenomas evade apoptosis via noxa deregulation in Cushing’s disease,” was published in the journal Cell Reports.
In Cushing’s disease, non-cancerous adenomas in the brain’s pituitary gland lead to the excess production and release of adrenocorticotropic hormone (ACTH). This triggers the adrenal glands, which sit atop the kidneys, to produce too much cortisol.
However, studies investigating the development of hormone-producing adenomas and the underlying mechanisms are lacking.
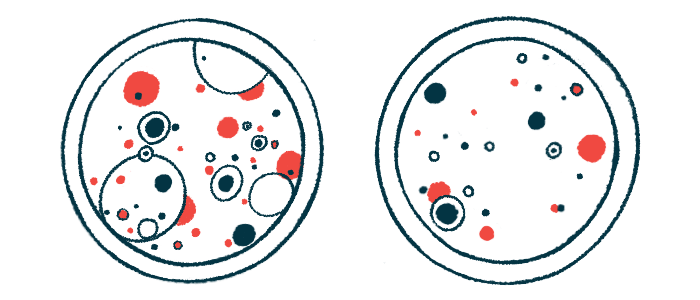
In this report, researchers at the National Institute of Neurological Disorders and Stroke in Maryland, analyzed the gene activity of individual cells in and around adenomas to characterize details of the tumor’s biology.
Adenomas and adjacent healthy tissue were collected from 34 patients via microsurgical dissection. From these, 24 had Cushing’s and one had subclinical Cushing’s (elevated cortisol levels, but without clinical signs). Those without Cushing’s had other conditions related to pituitary tumors.
Individual cells were separated, and 27,594 — including 15,513 cells from Cushing’s patients and 12,081 from non-Cushing’s patients — underwent gene activity analysis by RNA sequencing. Various cell types were identified by their specific genetic signatures.
Researchers then focused on tissue from three patients with sporadically occurring Cushing’s adenomas. Shared gene activity was identified by comparing ACTH-producing cells, called corticotrophs, from the core and margins of adenoma tissue.
Cushing’s signature genes
Among the genes that were more active at the adenoma core, but not in surrounding tissues — globally called Cushing’s signature genes — was POMC, which encodes for the prohormone precursor of ACTH. Other Cushing’s signature genes also included PMAIP1, PPP1R17, SPP1, PCSK1, and RSPO3.
Experiments confirmed that elevated PMAIP1 activity was specific to Cushing’s adenomas and not tumors related to other conditions. The PMAIP1 gene carries instructions for making a protein called noxa, which plays a role in apoptosis, or programmed cell death.
To understand the mechanisms underlying elevated PMAIP1 activity, the team examined patterns of chemical modifications that control gene activity. Some of the signature genes, including PMAIP1, had low levels of DNA methylation — a chemical modification in which methyl groups are attached to DNA to suppress gene activity. A lack of DNA methylation explained higher PMAIP1 activity, the team noted.
Notably, although PMAIP1 was more active, core Cushing’s adenoma cells had consistently low levels of noxa protein. This was not seen in adenomas from other conditions.
Researchers suggested that this discrepancy was due to the degradation of noxa by proteasomes — large protein complexes in cells that normally degrade damaged or unwanted proteins.
A corticotroph-enriched mouse cell line, which displayed many of the hallmarks of adenomas, such as elevated Pomc and Pmaip1 activity, was then created to investigate this.
Velcade’s role
Blocking the activity of the proteasome with an approved cancer medicine called bortezomib (sold under the brand name Velcade), effectively rescued noxa protein production. At the same time, bortezomib treatment lowered ACTH production, increased the levels of apoptosis markers, and reduced the survival of adenoma-like mouse cells.
At clinically relevant doses, bortezomib also suppressed the growth of adenoma cell lines derived from multiple Cushing’s patients, “demonstrating the therapeutic potential of proteasome inhibition in [Cushing’s disease]”, the team wrote.
Finally, investigators found that adenoma cell lines derived from non-Cushing’s patients required a higher dose of bortezomib to achieve the same growth suppression, “suggesting that the [Cushing’s disease] adenoma cells were more sensitive to noxa-mediated apoptosis.”
“We generated a [gene activity] map of the post-natal human pituitary gland and defined signature genes for [Cushing’s disease] adenomas,” the authors wrote.
“In addition, we identified apoptosis escape via proteasome-mediated noxa degradation,” they wrote. “Selective proteasomal inhibition rescued noxa and triggered apoptosis in human primary cells from [Cushing’s disease], suggesting its clinical utility for human [Cushing’s disease].”






