Fluorescent Pigment Builds Up in Cortisol-producing Tumors Associated with Cushing Syndrome, Study Reports
Written by |
Fluorescent pigments accumulate in the non-cancerous adrenal gland tumors associated with Cushing syndrome, whether or not a person has a mutation associated with the disease, a study indicates.
The build-up could be used a biomarker of Cushing disease some day, the researchers said.
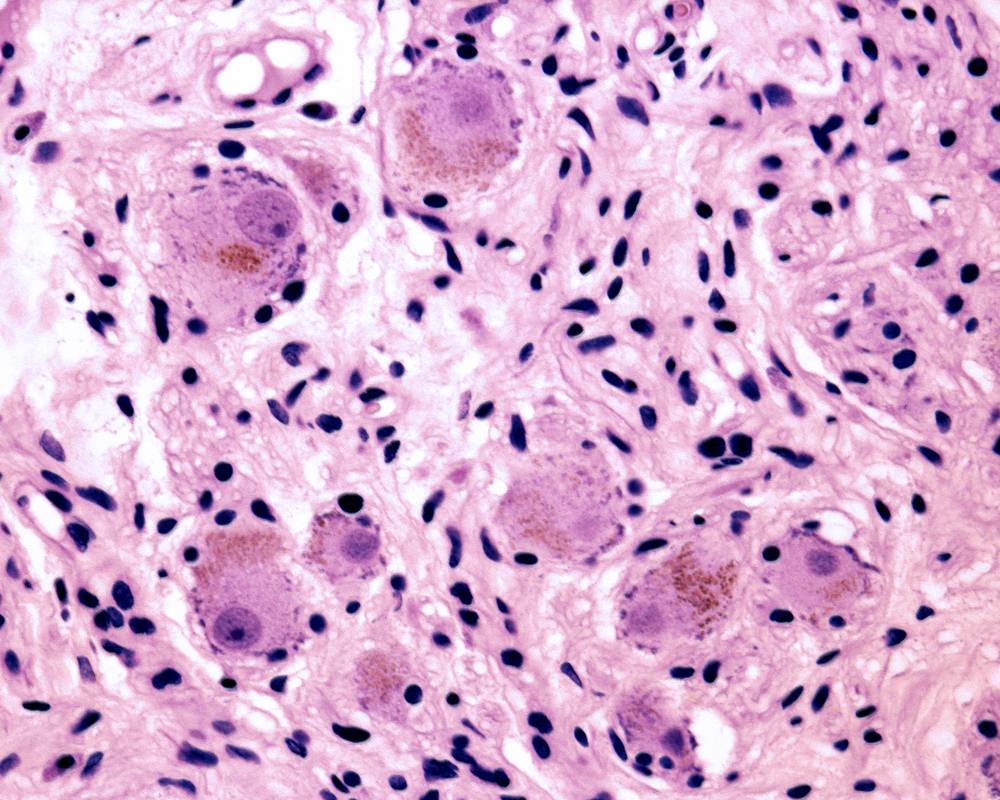
Scientists call the pigments lipofuscin granules. Granule accumulations increase with age, but this can also happen in adrenal gland tumors no matter what PRKACA mutation a person has, or even if there is no mutation, according to the study.
The research, “Lipofuscin Accumulation in Cortisol-Producing Adenomas With and Without PRKACA Mutations,” was published in the journal Hormone and Metabolic Research.
Lipofuscin is one of the products that remains in cells after organelles that dispose of cell waste, known as lysosomes, are themselves degraded.
Because liposfuscin cannot be degraded, liposfuscin granules accumulate with age. They build up in heart muscle cells, liver cells, brain neurons, and the adrenal glands as part of the normal aging process. The adrenal glands, which are located above the kidneys, produce hormones such as adrenaline and the steroids aldosterone and cortisol, excessive amounts of which are associated with Cushing syndrome.
The granules also accumulate in primary pigmented nodular adrenocortical disease, or PPNAD. That accumulation is responsible for the particular type of pigmentation that characterizes PPNAD.
PPNAD can lead to Cushing syndrome, in some cases due to mutations in genes that generate the PKA protein. Some of the Cushing’s mutations include PRKAR1A and PRKACA, which code for components of PKA. The mutations tend to trigger constant activation of PKA, leading to excess cortisol production.
Lipofuscin has no known function in adrenal-gland tumors. But researchers at the National Institutes of Health hypothesized that cortisol-producing adrenal-gland tumors with PKA gene defects accumulate more pigment than tumors that do not produce cortisol. This means that accumulations of the pigment could serve as a potential biomarker of cortisol production.
The team examined 10 tissue samples from patients with cortisol-producing tumors associated with Cushing syndrome. Four had a PRKACA mutation.
Researchers compared the samples with those of other adrenal-gland tumors, such as PPNAD lesions, which are known to accumulate lipofuscin, and with samples of Conn’s tumors, which don’t have the pigment.
The team found that cortisol-producing tumors had significantly more lipofuscin granules than adjacent tissue or Conn tumors. Interestingly, the presence of a PRKACA mutation did not significantly increase the amount of lipofuscin granules. This indicated that lipofuscin accumulates in all cortisol-producing tumors associated with Cushing syndrome.
Nonetheless, the researchers said that in PPNAD samples, PRKACA mutations led to a less intense accumulation of lipofuscin than PKRAR1A mutations. Since none of the patients in the study had faulty PRKAR1A, the most widely known mutation that causes Cushing’s syndrome, the team said that examining a larger patient population with PRKAR1A mutations might yield different results.





