Protocols lacking for reducing risk of VTEs in Cushing’s patients
Researchers collected data on 222 people diagnosed with condition in 2021-22
Written by |

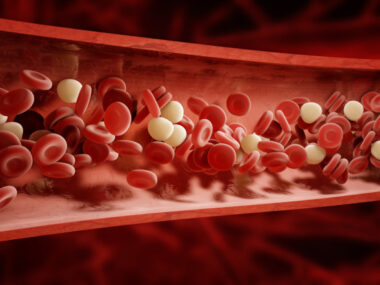
People with Cushing’s syndrome have an increased risk of venous thromboembolism (VTE), that is, dangerous blood clots that obstruct the normal flow of blood through veins, but most treatment centers don’t have standard procedures for reducing VTE risk in Cushing’s patients, a study indicates.
“A specific thromboprophylaxis protocol for patients with [Cushing’s syndrome] was not available in the vast majority of centers, despite the fact that retrospective cohort studies have shown a decrease in VTE-associated mortality and morbidity in patients with [Cushing’s syndorme] on anticoagulant [anti-clotting] treatment,” said the authors of “Venous thromboembolism in Cushing syndrome: results from an EuRRECa and Endo-ERN survey,” which was published in Endocrine Connections.
The researchers called for more studies to establish guidelines about how best to handle preventive anti-clotting treatment, or thromboprophylaxis, in Cushing’s.
Cushing’s syndrome is an umbrella term for conditions driven by excess levels of the hormone cortisol. Cushing’s disease is a specific form of the syndrome that’s caused by a tumor in the pituitary gland.
VTE is one of the major contributors for increased morbidity and mortality associated with Cushing’s. Although its incidence is much higher among Cushing’s patients than the general population, there’s no standardized protocol on how to prevent such events.
Managing risk of VTEs in Cushing’s
Here, researchers surveyed data from the European Registries for Rare Endocrine Conditions (EuRRECa), a tool established by centers that specialize in treating rare hormonal disorders, to learn more about the incidence and management of VTEs in Cushing’s.
The scientists collected data on 222 people diagnosed with Cushing’s in 2021 or early 2022. About two-thirds of them had Cushing’s disease, while the rest had other forms of the syndrome. Almost all underwent surgery and about a third were given cortisol-lowering medications.
The patients were followed at one of 20 centers in six countries (Spain, Italy, the Netherlands, Germany, Belgium, and Sweden). The researchers noted that six of the 20 treatment centers had a specific protocol in place for how to handle thromboprophylaxis in people with Cushing’s. Eleven other centers had a thromboprophylaxis protocol that wasn’t specific to Cushing’s and the other three had no protocol at all.
Along with the differences in protocols, there were differences about whether and how thromboprophylaxis was given. About two-thirds of patients received thromboprophylaxis at some point, though some started it before surgery and some afterward.
In almost all the cases, anti-clotting treatment used a class of medications called low-molecular weight heparins, but there were difference in how long thromboprophylaxis was maintained.
Among the patients with Cushing’s disease, thromboprophylaxis was often given to those who were older or had higher scores on measures of disease severity.
Guidelines needed for VTE risk
More studies were needed to establish clear guidelines for how best to reduce VTE risk in Cushing’s patients, the scientists said.
“Prospective clinical trials are needed to develop evidence-based guidelines on thromboprophylaxis,” they wrote.
Over a mean follow-up time of little more than a year, six (2.7%) patients had a documented VTE. In three of them, a VTE occurred despite thromboprophylaxis. The VTE proved to be fatal in one case.
Most patients who had VTE had other underlying conditions that are known to increase the risk of clotting problems, such as high blood pressure or a previous history of VTEs.
The incidence rate of VTE in this study was calculated to be at 14.6 per 1,000 person-years, meaning that if 1,000 people with Cushing’s were followed a year, it would be expected that 14 or 15 of them would have a VTE.
“We found … VTE occurred even in patients on cortisol-lowering medication and anticoagulants [anti-clotting medications],” wrote the researchers, who said more studies are needed about how to prevent this potentially fatal complication.