Some Pituitary Tumors May Increase Risk of Relapse After Surgery
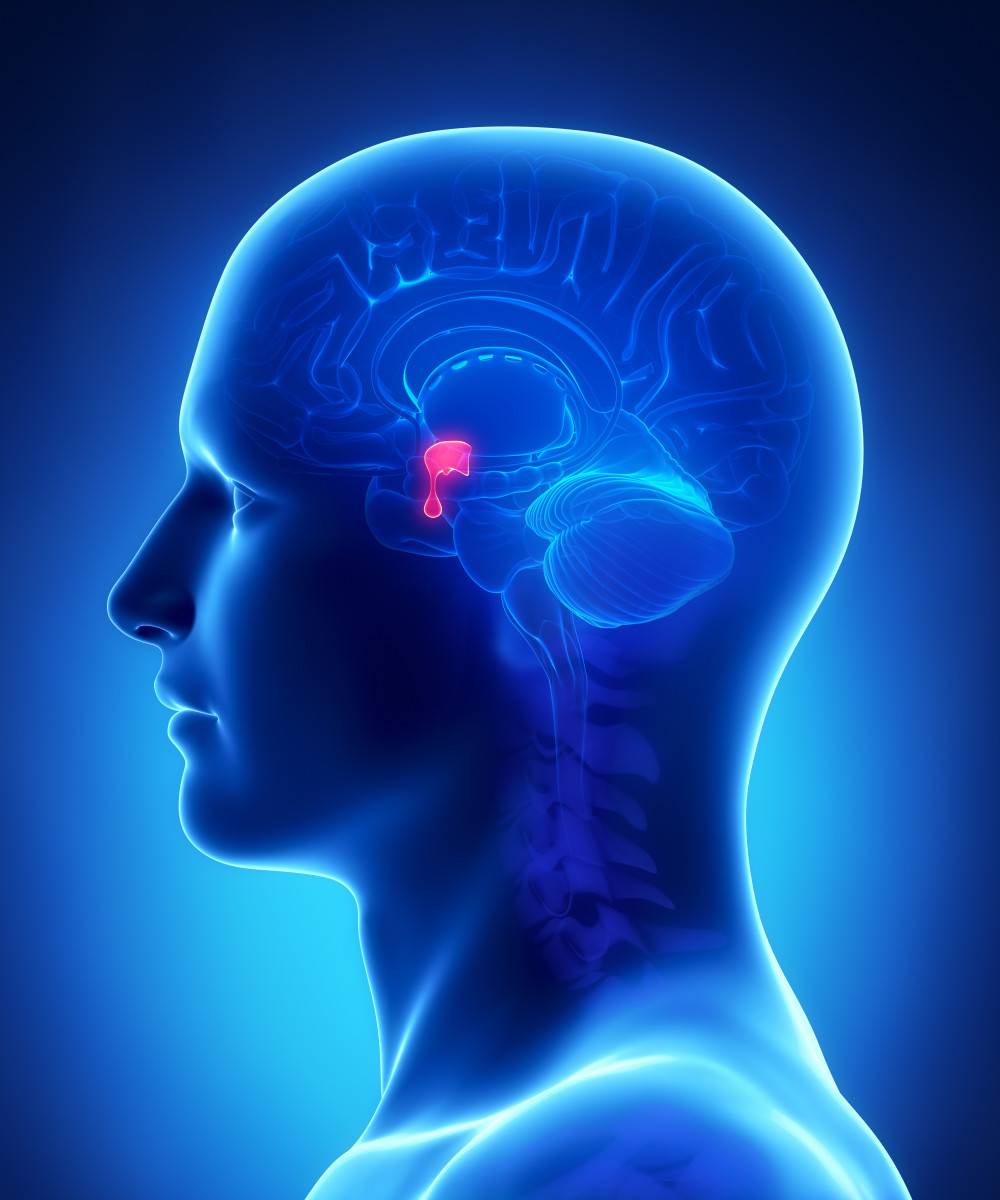
CLIPAREA l Custom media/Shutterstock
A type of tumor in the brain’s pituitary gland, which causes Cushing’s disease, has been found to be more invasive, and its presence lowers the likelihood of remission following surgery.
According to scientists, these study findings support the need to identify types of pituitary tumors to minimize post-surgical relapse.
The study, “Clinical, Biological, Radiological Pathological and Immediate Post-Operative Remission of Sparsely and Densely Granulated Corticotroph Pituitary Tumors: A Retrospective Study of a Cohort of 277 Patients With Cushing’s Disease,” was published in the journal Frontiers in Endocrinology.
Cushing’s disease is characterized by excessive levels of the hormone cortisol, which is produced and released by the adrenal glands sitting atop the kidneys.
Excess cortisol is triggered by the adrenocorticotropic hormone (ACTH), which is overproduced by the pituitary gland — found at the base of the brain — mainly due to the presence of benign (non-cancerous) tumors called adenomas.
Surgical removal of pituitary adenomas is the first-line standard treatment in Cushing’s. But due to high rates of relapse, extended follow-up is recommended as persistently elevated cortisol is associated with a higher risk of mortality.
Although pituitary adenomas are considered benign, different types of tumors can be more or less aggressive (invasive), with some being associated with a higher risk of relapse after surgery. Pituitary adenomas also can invade surrounding tissues, including those around the carotid arteries in the neck that supply blood to the brain.
However, the availability of reliable biomarkers to identify different types of pituitary tumors remains limited.
To find predictive biomarkers of tumor types related to invasiveness and disease relapse, researchers at the Medical University of Warsaw in Poland and their colleagues examined the medical records of patients who underwent pituitary surgery due to ACTH-dependent Cushing’s and assessed the clinical and tissue-related findings.
Investigators reviewed the records of 348 patients (278 women and 70 men) with a mean age of 43.45 years at diagnosis. Overall, pituitary tumors were found earlier in women than men (median 40 vs. 43.5 years). The time from symptom onset to surgery ranged from one to 20 years, with a mean of two years.
Extracted pituitary tissues were examined by electron microscopy and histology methods. In histology, tissues are stained with several dyes to distinguish different cell types and then examined under a standard microscope.
In samples from 277 patients, two types of tumors were identified: sparsely and densely granulated pituitary tumors.
Sparsely granulated (SG) tumors contained cells that were resistant to staining. A PAS stain, which interacts with carbohydrates, was faintly positive, and ACTH levels were low. These tumor cells had poorly developed internal structures and did not contain protein fibers around the nuclei — the cell compartments where genetic information is stored.
In contrast, densely granulated (DG) tumors had cells that showed strong positive PAS staining and high ACTH production. Internal cell structures were numerous and larger, with the presence of protein fibers around the nuclei.
Both of these cell types were found predominately in women, with both occurring at a similar age. Densely granulated tumors accounted for the majority of microadenoma cases (tumors measuring less than one centimeter in diameter).
MRI scans taken before surgery were used to establish tumor invasiveness through Knosp’s scale grades, which range from 0 to 4. A grade of 0 refers to tumors located within the pituitary gland, while a grade of 4 represents those that have grown and invaded surrounding tissues.
MRI scans were available for 243 cases among participants with an established granularity pattern.
There was an increased frequency of SG tumors in patients with higher Knosp’s scale grades (2 to 4). Tumor volumes also were higher in patients with SG versus DG tumors.
Additionally, invasiveness — defined as a Knosp’s grade of 2 or more — was more frequent in SG tumors. These tumors also had a significantly higher Ki-67 proliferation index, or greater ability to spread, compared with DG tumors.
Moreover, patients with SG tumors had higher blood cortisol levels in the first five days following surgery compared with those who had DG tumors (median of 6.52 mcg/dL vs. 2.49 mcg/dL). Notably, those with DG tumors more frequently achieved a remission status — defined as blood cortisol levels lower than 2.0 mcg/dL.
“We highlight the importance of granularity pattern among corticotroph pituitary tumors, since the SG phenotypes [characteristics] correlate with more invasive features such as higher Knosp’s scale grades, bigger tumor volumes, and higher Ki-67 proliferation index,” the researchers wrote.
“But yet, SG phenotypes are less frequently prone to achieve an immediate remission status,” they wrote, adding these findings “justify the need for an accurate differentiation of DG and SG subtypes.”





