ACTH/Cortisol Ratio May Be Simple, Reliable Test to Diagnose Cushing’s Disease
Written by |
The ratio between adrenocorticotropic hormone levels and cortisol levels in the blood is higher among Cushing’s disease patients than in healthy people, a new study has found, suggesting that measurement could be used to help diagnose the disease.
Also, higher values at diagnosis could predict if the disease will recur and indicate larger and more invasive tumors.
The research, “The Utility of Preoperative ACTH/Cortisol Ratio for the Diagnosis and Prognosis of Cushing’s Disease,” was published in the Journal of Neurosciences in Rural Practice.
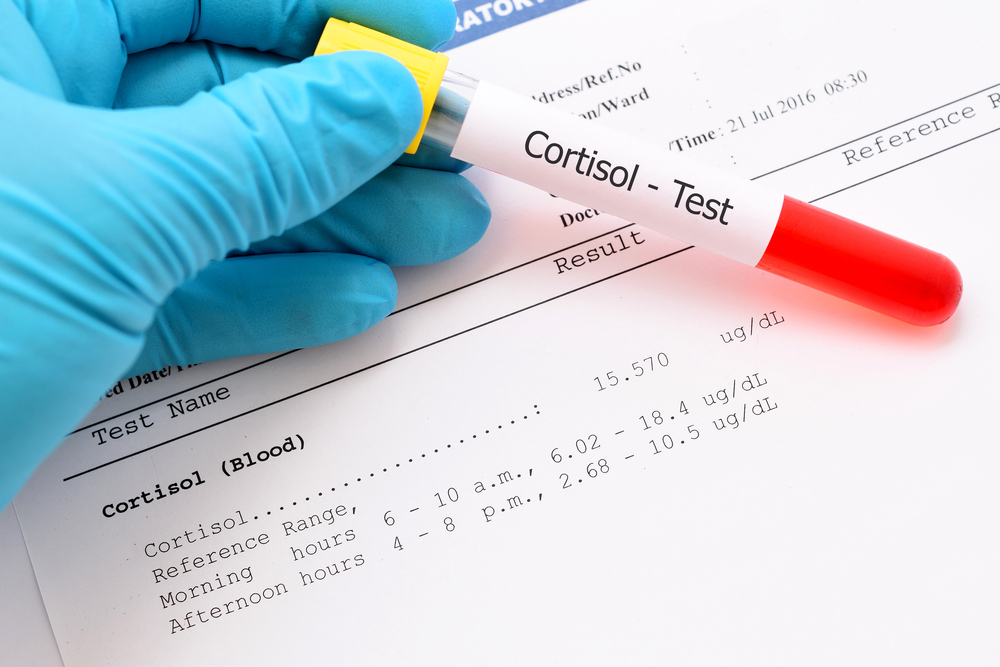
Cushing’s syndrome (CS) is characterized by excess levels of cortisol. In patients with suspected CS, clinicians recommend testing late-night salivary or plasma (blood) cortisol, 24-hour urine-free cortisol (UC), as well as morning cortisol levels after low-dose suppression with dexamethasone, a corticosteroid.
CS may be ACTH-dependent or ACTH-independent, meaning that the high cortisol levels are caused by excess ACTH production.
Patients with CD have elevated levels of ACTH. A tumor, usually an adenoma, causes the pituitary gland to produce excess levels of ACTH, which stimulate the release of cortisol from the adrenal glands. Cortisol usually inhibits ACTH production. However, in CD patients, this feedback mechanism is absent.
Despite extensive research and clinical data, the variable and usually nonspecific signs and symptoms of CD still represent relevant challenges for diagnosis. Clinical manifestations must be associated with biochemical tests, which often have led to conflicting results.
Studies showed that although ACTH levels correlate with the size of the pituitary adenoma, the levels of cortisol do not increase as much. In fact, lower cortisol/ACTH ratios have been reported in patients with macroadenoma – which is greater than 10 millimeters in size – than in those with microadenoma, which is smaller than 10 millimeters.
Conversely, the research team hypothesized that besides their utility for determining the cause of CS, the inverse ratio – ACTH/cortisol – also may be useful for diagnosis.
The team evaluated the pretreatment plasma ACTH/cortisol levels in CS patients with excess cortisol production due to abnormal pituitary or adrenal function. Data from patients were compared with that of individuals without CS.
The study included 145 CS patients diagnosed from 2007 to 2016, 119 patients with CD, 26 with ACTH-independent CS (AICS), and 114 controls with no CS.
Patients’ clinical, laboratory, imaging, postsurgical and follow-up data were analyzed.
Results showed that patients with CD had a significantly higher basal ACTH/cortisol ratio than controls or those with AICS.
“These results showed ACTH/cortisol ratio might be a simple and useful test for the diagnosis of ACTH-dependent CS,” the researchers wrote.
Importantly, the scientists observed that a ACTH/cortisol ratio above 2.5 indicated identified 82 percent of positive CS cases and 63 percent of controls.
Overall, “an ACTH/cortisol ratio [greater than] 2.5 would be beneficial to diagnose CD together with other diagnostic tests,” they concluded.
Patients with recurrent CD showed higher pretreatment ACTH levels and ACTH/cortisol ratio than those who achieved sustained remission. CD patients also exhibited more invasive, atypical and larger tumors, as well as lower postoperative remission and higher recurrence rates.
“Higher ACTH/cortisol ratio might predict poorer prognosis,” the investigators said.





