Effective treatment found to ease depression, anxiety in Cushing’s
But researchers say 'meaningful recovery' is incomplete for some patients
Effective treatment, either surgical or using medications, significantly eased anxiety and depression, and improved quality of life, in some people with Cushing’s syndrome, according to the findings of a new U.S. study.
However, when looking at treatment type, only patients who underwent surgery to remove tumors showed a statistically significant improvement in quality of life, and less depression and anxiety. Those treated with medication experienced a significant improvement only in measures of anxiety, the data showed.
According to the researchers, “although effective treatment improves mood and [quality of life in Cushing’s], clinically meaningful recovery is variable and incomplete for some patients.”
As such, these results support a model of care that goes beyond cortisol reduction, and also integrates “psychosocial follow-up and individualized treatment” for people with Cushing’s syndrome who experience impairments in quality of life and mood, the researchers wrote.
The study, “Prospective Assessment of Mood and Quality of Life in Cushing syndrome before and after Biochemical Control,” was published in The Journal of Clinical Endocrinology & Metabolism.
Cushing’s syndrome refers to conditions that result from elevated cortisol, or hypercortisolism, frequently caused by tumors in the pituitary gland. Such tumors produce excess adrenocorticotropic hormone (ACTH), and in these cases, the condition is known as Cushing’s disease. The syndrome can also result from ACTH-secreting tumors in other organs — then known as ectopic Cushing’s — or tumors in the adrenal glands, where cortisol is produced.
Cushing’s is tied to multiple other conditions, including depression and anxiety
Cushing’s has been associated with multiple coexisting conditions, or comorbidities, including depression and anxiety, that can significantly affect patients’ quality of life.
To learn more about these ties, a research team from Memorial Sloan Kettering Cancer Center in New York conducted a real-world study that sought to evaluate changes in quality of life, depression, and anxiety in people with Cushing’s, before and after achieving normal cortisol levels.
A total of 67 patients treated at the medical center were enrolled in the study. These individuals had a mean age of 42.3, and most — 84% — were women. Among them, 60 had Cushing’s disease, while seven were diagnosed with adrenal Cushing’s.
The participants were followed for a mean of 2.3 years, and a maximum of 11.5 years. At baseline, or the beginning of the study, all had elevated levels of blood and salivary cortisol and ACTH. The most common co-occurring at baseline were high blood pressure (82.1%) and diabetes (41.8%) or pre-diabetes (22.4%).
At the most recent follow-up, about two-thirds of the patients had been treated with transsphenoidal surgery, a minimally invasive procedure to remove pituitary tumors. The disease was being controlled with medication for slightly more than one-quarter of patients. Ten individuals had undergone surgical removal of one or both adrenal glands.
Among the medications used at the last follow-up were Isturisa (osilodrostat), taken by 44% of patients, metyrapone, given to one-third, and ketoconazole, prescribed for 22%.
Hydrocortisone replacement therapy, used to replace cortisol, often due to temporary or permanent adrenal insufficiency, was administered at 30 different follow-up visits throughout the study.
At the longest follow-up, there was a significant reduction in cortisol levels, as well as a decrease in the proportion of patients with diabetes and hypertension, according to the researchers.
Surgical treatment appeared to be more effective than medications
The patients’ quality of life was assessed using the Cushing QoL, a validated disease-specific questionnaire that evaluates physical and psychological issues. In this measure, higher values represent better quality of life.
At the last follow-up, treatment had led to a mean overall improvement in quality of life by 18.2 points. Gains were seen particularly among those who underwent transsphenoidal surgery versus receiving medical therapy (20 vs. 12.1 points).
Treatment also led to an easing of patients’ depression and anxiety, the researchers noted.
When assessed by treatment strategy, surgery resulted in significant improvements across quality of life, depression, and anxiety, whereas medical therapy only resulted in a significant easing of anxiety, the data showed.
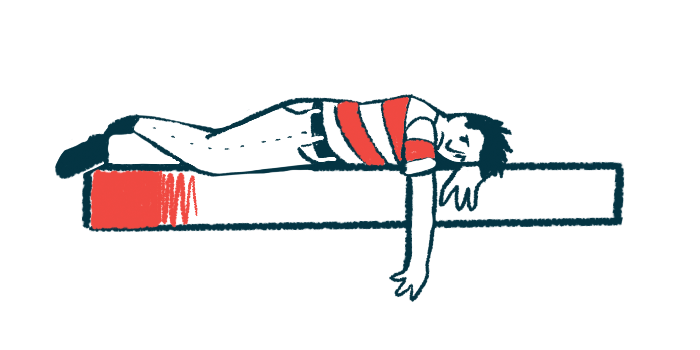
One-third to one-half of patients do not experience clinically meaningful improvements in … measures [of depression or anxiety, or indicators of quality of life].
Overall, a clinically meaningful difference was achieved in 65% of patients for quality of life, 68% for depression, and about 53% for anxiety. According to the researchers, this demonstrates that “one-third to one-half of patients do not experience clinically meaningful improvements in these measures.”
Further analysis revealed several factors tied to clinically meaningful improvement in quality of life. One was a lower body mass index (a measure of body fat using a ratio of weight to height) at baseline, while another was experiencing symptoms for less than three years prior to diagnosis. Hydrocortisone replacement therapy for longer than six months and normal salivary cortisol levels after treatment were also tied to clinically meaningful quality of life gains.
Additionally, easing of depression was associated with a symptom duration of less than three years before diagnosis, normal cortisol levels, and surgical treatment, while a reduction in anxiety was predicted by a younger age and more than six months of hydrocortisone replacement therapy.
“We identified predictors of improvement that highlight the need for early detection of [Cushing’s syndrome] and treatment strategies that allow for recovery of cortisol circadian rhythm,” the researchers wrote. Circadian rhythm refers to the body’s natural 24-hour cycle that affects functions such as hormone release, including cortisol.
“Our findings support a model of care that extends beyond [cortisol reduction],” the team concluded.