Detailed MRI Analysis Provides Correlations with Clinical Features and Response to Treatment in Cushing’s Disease, Study Shows
Written by |
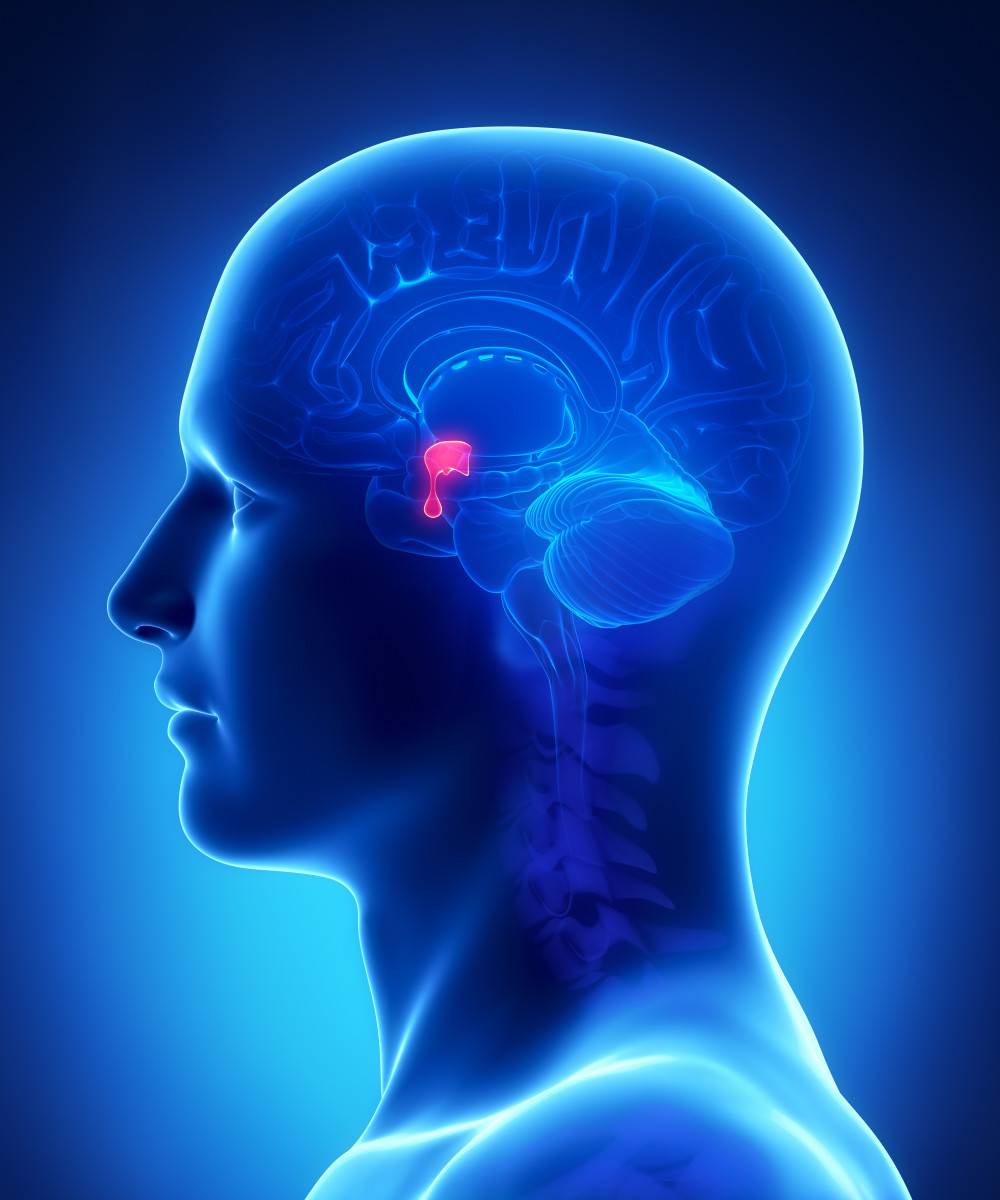
CLIPAREA l Custom media/Shutterstock
Detailed imaging analysis of patients with Cushing’s disease (CD) and other disorders caused by pituitary adenomas (tumors that arise from the pituitary, a small gland in the brain) provides correlation with clinical characteristics and treatment response, a new Turkish study reports.
The research, “Clinicopathological significance of baseline T2-weighted signal intensity in functional pituitary adenomas,” appeared in the journal Pituitary.
Diagnosis of pituitary adenomas is often done with magnetic resonance imaging (MRI), which provides data on the tumor’s localization, its invasiveness, as well as cell death and other changes. However, MRI does not enable precise evaluation of the tumor’s hormone production and behavior.
Studies on T2-weighted signal intensity (T2-WSI) — one of the basic parameters in MRI scans that highlights fat and water in the body — shows that it correlates with collagen content, degree of fibrosis (scarring), amyloid protein accumulation, and granulation pattern of somatotroph adenomas, which produce excessive levels of growth hormone, causing acromegaly (a hormonal disorder that results from too much growth hormone in the body).
Evaluation of granulation patterns is key in predicting response to somatostatin analogues (SSAs) treatment, the researchers observed. SSAs are intended to stop excess hormone production.
In contrast, analysis of T2-WSI in corticotroph adenomas — benigh tumors typical in Cushing’s disease patients that release elevated levels of adrenocorticotropin (ACTH) – is still lacking.
The research team assessed the correlation of T2-WSI with clinical features, granulation patterns, and response to treatment in patients with functional pituitary adenomas (FPAs), which are collectively characterized by excessive production of one or more hormones.
Specifically, scientists focused on 29 patients with Cushing’s disease, 87 with acromegaly, and 78 with prolactinoma, a type of benign pituitary tumor that produces elevated amounts of prolactin.
Results showed that while most somatotroph adenomas (53%) were hypointense, which means a darker image on MRI, the majority of prolactinomas (55%) and corticotroph adenomas (45%) were at least generally hyperintense, meaning lighter on image.
Data also revealed that hyperintense somatotroph adenomas were larger, sparsely granulated, and exhibited reduced shrinkage after treatment with SSAs.
In contrast, hypointense tumors were associated with higher levels of baseline insulin-like growth factor (IGF)-1% ULN, a predictor of insulin sensitivity, and a better response to SSAs.
In women with prolactinomas, hyperintensity correlated with smaller tumor diameter. In turn, hypointense prolactinomas were linked with younger age at diagnosis, higher baseline prolactin levels, and resistance to treatment with a dopamine agonist.
Scientists also found that hyperintense corticotroph adenomas correlated with larger tumor size and a sparsely granulated pattern. No difference was found between hyper and hypointense adenomas on cortisol and ACTH levels.
Investigators also reported that T2-WSI was not correlated with better surgical outcomes or with recurrent Cushing’s disease. Analysis of tumor shrinkage in these patients was not possible, the researchers noted.
“Although in present there is no immediate clinical application, we believe that if medical shrinkage of corticotrophs ever became a part of clinical practice, similar analyses could be performed in the future,” the researchers wrote.
“Further studies with larger series are required in order to make stronger suggestions,” they added.





