Night Cortisol Levels for Diagnosing Cushing’s Syndrome Less Accurate in Clinical Practice, Study Finds
Written by |
Salivary cortisol levels can be used to diagnose Cushing’s syndrome with relatively high reliability, but each test center should establish its own measurement limits depending on the exact method used for the test, a study from Turkey shows.
Researchers, however, caution that late-night salivary cortisol measurements in clinical practice is likely to be less accurate than that seen in controlled studies, and some patients might require additional tests for a correct diagnosis.
The study, “Diagnostic value of the late-night salivary cortisol in the diagnosis of clinical and subclinical Cushing’s syndrome: results of a single-center 7-year experience,” was published in the Journal of Investigative Medicine
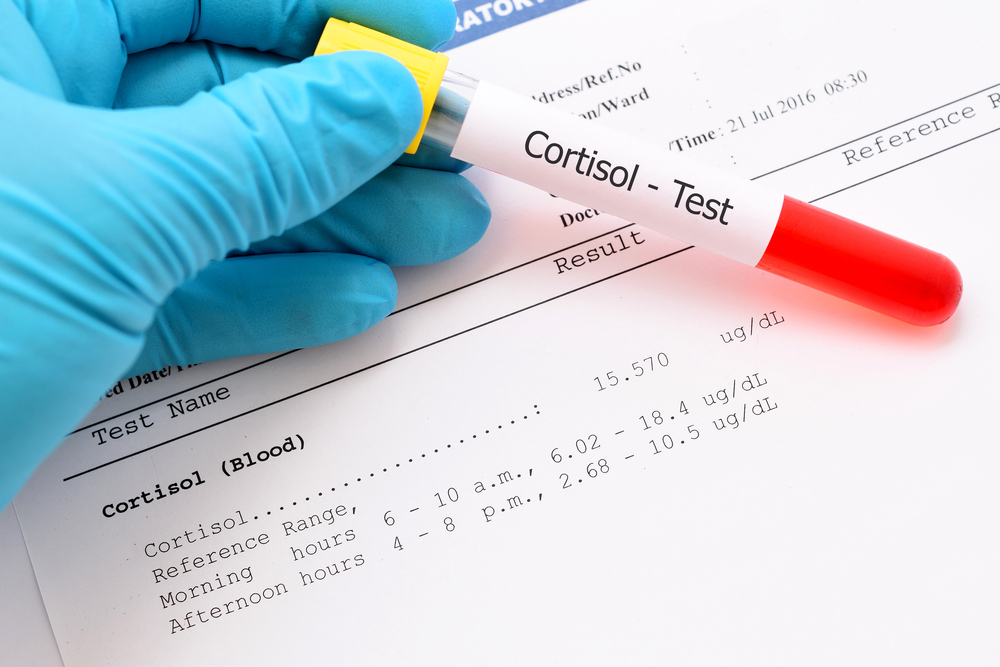
In healthy individuals, the levels of cortisol — a steroid hormone secreted by the adrenal glands — go through changes over a 24-hour period, with the lowest levels normally detected at night.
But this circadian rhythm is disrupted in certain diseases such as Cushing’s syndrome, where night cortisol levels can be used as a diagnostic tool.
Among the tests that can be used to detect these levels are late-night serum cortisol (LNSeC) and late-night salivary cortisol (LNSaC) tests. Since it uses saliva samples, LNSaC is more practical and does not require hospitalization, so it is often recommended for the diagnosis of Cushing’s syndrome.
So far, though, there has been no consensus regarding cutoff values and the sensitivity of the test.
Mustafa Kemal Balci, MD, and his team at the Akdeniz University in Turkey aimed to evaluate the diagnostic use of LNSaC in patients with clinical Cushing’s syndrome and in those with subclinical Cushing’s syndrome — people with excess cortisol but without signs of the disease.
The study involved 58 patients with clinical Cushing’s syndrome (CCS), 53 with subclinical Cushing’s syndrome (SCS), and 213 patients without Cushing’s syndrome who were used as controls.
Saliva and serum cortisol levels were measured in all patients, and statistical tests were used to study differences in these levels among the three groups of patients.
In CSC patients, the median cortisol levels were 0.724 micrograms per deciliter of blood (µg/dL), which dropped to 0.398 and 0.18 in patients with subclinical disease and controls.
The optimal cutoff point to distinguish patients with clinical Cushing’s was set at 0.288 µg/dL, where 89.6% of patients identified as positive actually have the disease (sensitivity), and 81.6% of patients deemed as negative were without the disease (specificity).
With a lower cutoff point — 0.273 µg/dL — researchers were also able to identify patients with subclinical disease with high sensitivity and specificity.
While the test showed high sensitivity and specificity values for clinical Cushing’s syndrome, its diagnostic performance was lower than expected in daily clinical practice, researchers said.
“The diagnostic performance of late-night salivary cortisol in patients with subclinical Cushing’s syndrome was close to its diagnostic performance in patients with clinical Cushing’s syndrome,” researchers wrote.
However, regarding the application of this test in other centers, they emphasize that “each center should determine its own cut-off value based on the method adopted for late-night salivary cortisol measurement, and apply that cut-off value in the diagnosis of Cushing’s syndrome.”





