Low Muscle Mass, High Visceral Fat Correlate With Disease Severity in Cushing’s Patients
Lower muscle mass and higher visceral fat are correlated to higher cortisol levels, and can be used as reliable biomarkers to assess disease severity in patients with adrenal adenomas, a new study shows.
The study, “Impact of hypercortisolism on skeletal muscle mass and adipose tissue mass in patients with adrenal adenomas,” was published in the journal Clinical Endocrinology.
Cushing’s disease and adrenal tumors can lead to high levels of cortisol. However, the percentage of patients with high cortisol levels is low (0.7-5 percent) and most tumors are NFATs (non-functioning adrenal tumors) and do not lead to the production of excess hormones.
The remaining 47 percent of patients with adrenal tumors have mild autonomous cortisol excess (MACE).
Patients with MACE tend to have a higher prevalence of cardiovascular risk factors, such as hypertension, type 2 diabetes mellitus, obesity, and abnormal lipid levels (dyslipidemia).
When patients with MACE undergo adrenalectomy (removal of the adrenal glands), they experience a decrease in cardiovascular risk factors. Unfortunately, selecting patients who might benefit from adrenalectomy is difficult. That is why a reliable biomarker that can inform which patients are at a higher risk for cardiovascular disease would be better for management of MACE.
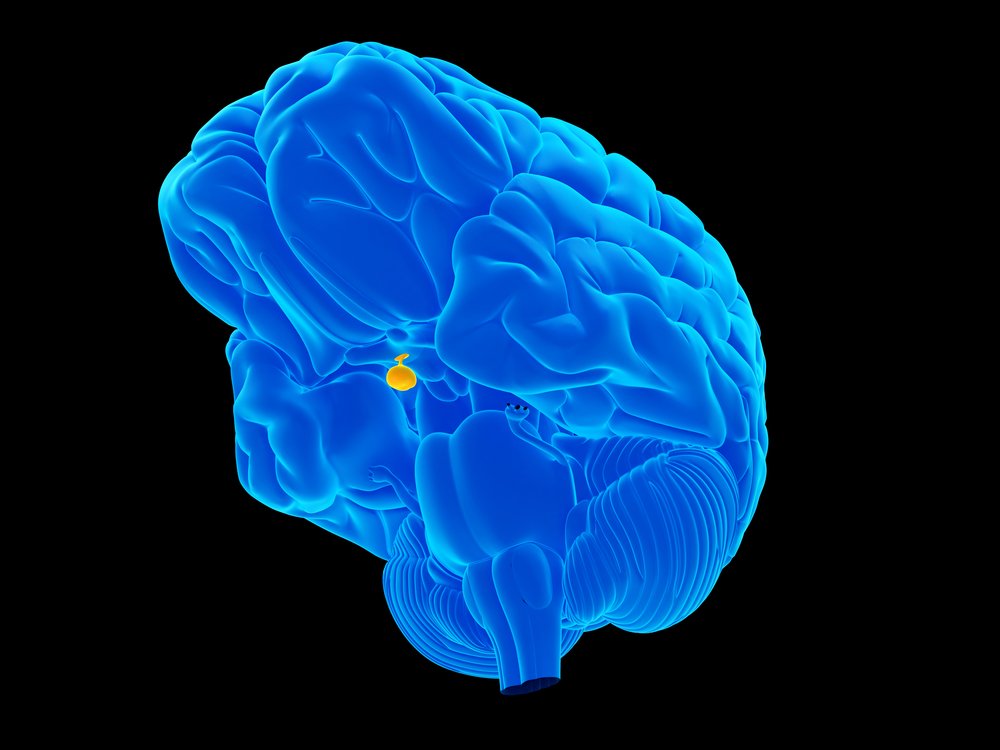
High levels of cortisol lead to an increase in visceral abdominal adiposity, referring to the fat that resides on the organs of the abdomen, as well as an increase in muscle loss, referred to as central sarcopenia. However, little is known about the cortisol-induced changes in the bodies of patients with adrenal adenomas and MACE.
Researchers hypothesized that changes in body composition in patients with MACE, Cushing’s syndrome, and NFAT could be related to degrees of cortisol excess.
To test their hypothesis, they reviewed medical records and measured body composition, including levels of visceral fat [VAT], subcutaneous fat [SAT], visceral/total fat [V/T], visceral/subcutaneous [V/S], and total abdominal muscle mass. Visceral fat around organs is “deeper” than subcutaneous fat, which is closer to the skin.
Results showed that patients with Cushing’s syndrome, compared to NFAT patients, had an increased V/T ratio and V/S ratio. Furthermore, total muscle mass was reduced by 10 cm2 in patients with Cushing’s compared to patients with NFAT.
Interestingly, patients with MACE had a decrease in V/T ratio and V/S ratio compared to patients with NFAT.
Researchers then correlated cortisol levels, as determined by a standard dexamethasone suppression test, with the body composition parameters. Results showed that for every 28 nmol/L cortisol increase, there was a 0.008 increase in V/T, 0.02 increase in the V/S fat ratio, and a 1.2 cm2 decrease in mean total muscle mass.
In other words, the higher the cortisol levels, the higher the visceral fat, and the lower the muscle mass.
As both visceral fat and lower muscle mass are correlated to cardiovascular risk, they could serve as reliable biomarkers.
“We propose the measurements of body composition as a potential noninvasive test,” the researchers concluded.
However, “performing body composition analysis in a larger sample of well-characterized patients with adrenal adenomas, not limited to patients undergoing adrenalectomy, is necessary before transformation of such biomarker into clinical practice,” they added.






