Cushing’s Syndrome Sometimes Caused by Abnormal Receptors on Adrenal Glands, Case Report Shows
In rare cases, abnormal receptors on the adrenal glands can cause excess cortisol and Cushing’s syndrome, according to a case report.
Identifying these receptors can allow physicians to treat the disease pharmacologically rather than surgically, the researchers say.
The report, “Two cases of Cushing’s syndrome due to primary bilateral macronodular adrenal hyperplasia secondary to aberrant adrenal expression of hormone receptors,” was published in the journal Clinical Biochemistry.
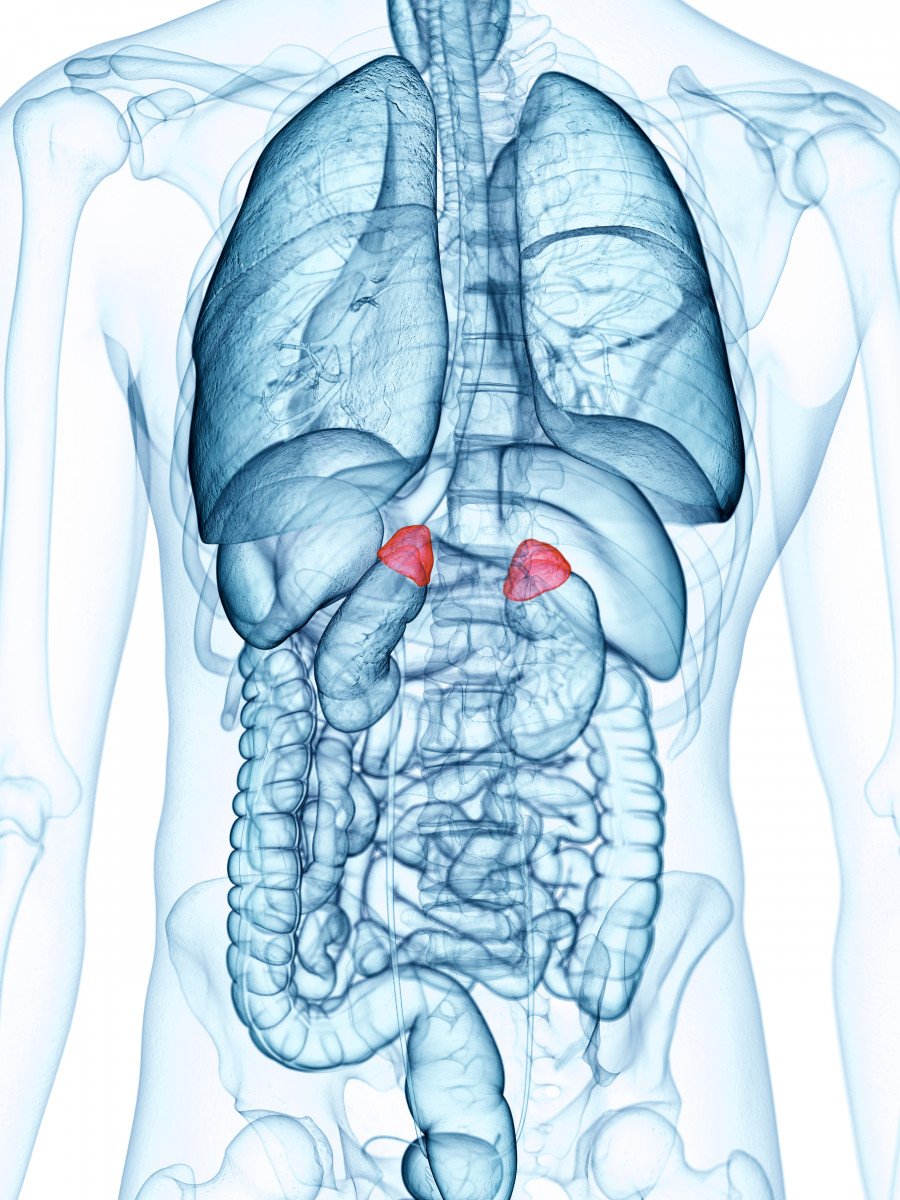
Adrenocorticotropic hormone (ACTH) stimulates the adrenal glands to release a hormone called cortisol. Most cases of Cushing’s syndrome (CS) are attributed to excess ACTH, leading to high cortisol levels.
In about 15-20 percent of cases, however, high cortisol levels are caused by mechanisms independent of ACTH. While these are mostly caused by tumors, in less than 1 percent of cases, ACTH-independent CS is caused by bilateral macronodular adrenal hyperplasia (BMAH) — a disease characterized by nodules on both adrenal glands.
The adrenal gland has receptors for a range of hormones, many of which are involved in the production of steroids — such as cortisol. An abnormal increase in any of these receptors can lead to high levels of cortisol, which is the case for patients who have BMAH. The challenge in effectively treating the disease, however, is to determine which receptors are over-produced.
In this report, researchers presented the case of two patients with Cushing’s syndrome due to BMAH. The goal of this study was to detect the receptors responsible for the excess cortisol using an extensive screening protocol.
Researchers used a modified version of the previously published Lacroix protocol in which they conducted measurements of ACTH, cortisol, and other steroids and hormones. They then had the patients do an upright posture test, where they went from lying down on their left side to standing, as well as giving them a mixed meal and administering gonadotropin-releasing hormones (GnRH) to serve as stimulation.
The mixed food was given to determine whether the increase in cortisol was due to gastrointestinal hormone-mediated steroid production. GnRH was given to see if the GnRH receptor was responsible for over-production of cortisol.
Additionally, both patients were stimulated by ACTH injected into the vein to determine whether the cortical response was dependent or independent of ACTH.
A positive response was defined as any increase in cortisol above 50%, a partial positive response was between 25-49%, and any increase below 25% was considered a negative response.
The first case, a 69-year old man, did not respond to ACTH administration, ruling out the possibility that the cortisol changes could be attributed to ACTH. Additionally, he had a negative response to standing and mixed meal stimuli.
Interestingly, the patient had a 36.5% response to GnRH administration, indicating a partial response to this hormone. This suggests there was an abnormal expression of the receptors for GnRH on the adrenal gland.
The second case, a 53-year old woman, was admitted to the department of endocrinology and evaluated for CS. She had high cortisol levels, but essentially no detectable ACTH, ruling out the possibility that CS was due to ACTH over-production. She also had a negative response to the mixed meal and GnRH stimuli.
Interestingly, the woman had a partial positive response (41.9%) to the upright posture test, suggesting high levels of receptors for the hormone vasopressin V1, which increases in response to changes in posture. The abnormal activation of vasopressin V1 receptors, in turn, produce high levels of cortisol.
In both cases, researchers were able to identify the receptors responsible for cortisol excess. While both patients were treated by undergoing an adrenalectomy, or removal of the adrenal gland, medications that target these receptors could also be used.
“The cases presented exemplify the importance of studying anomalous receptors in patients affected by ACTH-independent Cushing’s syndrome with bilateral adrenal affectation, allowing the possibility of using pharmacological treatments as an alternative to adrenalectomy,” the investigators concluded.






