Medication for abdominal pain triggers Cushing’s in woman, 62
Long-term treatment with corticosteroids can lead to syndrome: Report

The prolonged use of an injectable medication containing an anti-inflammatory corticosteroid to treat abdominal pain led to the onset of Cushing’s syndrome in a 62-year-old woman, as described in a case reported by a team in Florida.
The woman was being treated for pain associated with chronic inflammation in the pancreas, according to the researchers, who said her case highlights the need for both patients and clinicians to be aware of the potential adverse effects that can occur “with excess of glucocorticoid activity.”
“Treatment with corticosteroids can lead to iatrogenic [drug-induced] Cushing’s syndrome when used for longer intervals and in high doses,” the researchers wrote, adding that “patients undergoing treatment with therapeutic doses of corticosteroids should be regularly and thoroughly counseled about the potential adverse effects of prolonged use.”
The report, “A case of celiac plexus block causing iatrogenic Cushing’s syndrome,” was published in the journal Clinical Case Reports.
Woman given medication cocktail — with corticosteroid — for abdominal pain
Cushing’s syndrome comprises a group of conditions marked by high levels of the stress hormone cortisol, which is also referred to as hypercortisolism. One of its more common subtypes, Cushing’s disease, is caused by a tumor in the brain’s pituitary gland.
However, Cushing’s also may arise as a side effect of certain medications, such as corticosteroids. In such cases, it is called iatrogenic, or drug-induced, Cushing’s syndrome.
Corticosteroids are a class of anti-inflammatory and immunosuppressive medications that work by mimicking cortisol’s activity. They are often used to treat autoimmune disorders or inflammatory conditions. However, high levels of corticosteroids in the body for a prolonged period of time may lead to the onset of Cushing’s syndrome.
In this report, researchers at the Mayo Clinic in Jacksonville, Florida, described the case of a woman with abdominal pain who developed Cushing’s syndrome after using an injectable medication cocktail. She used that cocktail, containing a corticosteroid, for a long period of time to manage pain associated with chronic pancreas inflammation.
The woman was referred to Mayo due to a recent onset of fatigue, weakness, and decreased appetite. She also reported a history of weight gain and muscle pain.
Her past medical history included recurrent pancreas inflammation, known as pancreatitis, gastroesophageal reflux disease, high blood pressure, and high levels of fatty molecules in the blood. She also had a history of migraines.
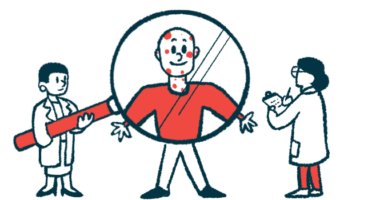
A physical examination revealed the woman had high blood pressure and was obese. Over the prior four months, she had gained 5.5 kg (about 12 pounds).
She also had several symptoms indicative of Cushing’s, such as facial redness and a buildup of fat between the shoulder blades, and in the upper back and abdomen. She also reported easy bruising, although no bruises were visible at the time of the examination.
Blood tests revealed the patient had low levels of cortisol and adrenocorticotropic hormone (ACTH), a signaling molecule that regulates cortisol production.
No evidence of prescribed corticosteroids found in case history
A comprehensive review of her medication history showed no evidence of prescribed corticosteroids, and the patient denied the use of medications containing corticosteroids.
However, further discussions with her medical teams revealed she had been receiving — every few months for the prior two years — an injectable medication cocktail to manage abdominal pain associated with chronic pancreatitis. That cocktail contained triamcinolone acetonide, a corticosteroid, and bupivacaine, a potent local anesthetic.
“The patient was not aware that these injections contained corticosteroids and of the potential associated side effects,” the researchers wrote.
Three months later, repeat testing demonstrated that the woman’s cortisol and ACTH levels were both within the normal range.
The patient was counseled on the side effects associated with prolonged exposure to high doses of corticosteroids and advised to discuss with her medical team the possibility of decreasing the dose or frequency of medication for her abdominal pain to prevent these effects.
The patient was not aware that these injections contained corticosteroids and of the potential associated side effects. … Less common administration routes may conceal the exposure, raising the possibility of misdiagnosis and mismanagement.
“When suspected clinically, a thorough inquiry regarding corticosteroid therapy should be conducted to confirm the correct diagnosis of iatrogenic hypercortisolism,” the researchers wrote.
The team noted that “less common administration routes may conceal the exposure, raising the possibility of misdiagnosis and mismanagement.”
This case highlighted that patients should be informed if they are receiving treatments containing corticosteroids, and advised on the potential side effects associated with the prolonged use of such medications, according to the researchers.