FAQs about Isturisa
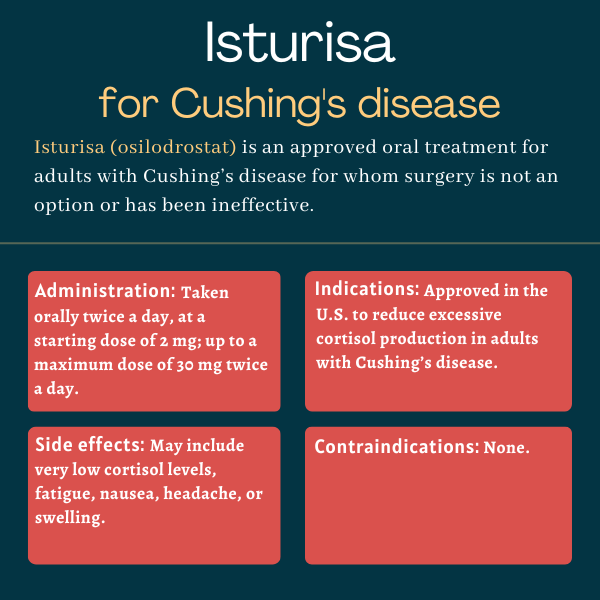
Isturisa was approved by the U.S. Food and Drug Administration (FDA) in 2020 for adults with Cushing’s disease who are not eligible for pituitary surgery or for whom the procedure was not effective.
There are no known interactions between Isturisa and alcoholic beverages. However, using alcohol while taking some medications can reduce their effectiveness or cause side effects. Patients wishing to drink while using Isturisa should discuss such preferences with their healthcare providers.
In the LINC-3 clinical trial that supported Isturisa’s approval, the median time to first complete response was reported to be 41 days, meaning that some patients may see their cortisol levels drop within a few months after starting with Isturisa. However, every patient is different and the time it takes for a treatment response can vary. Patients are advised to talk with their doctors about how Isturisa can help in their individual case.
The most common side effects of Isturisa include low cortisol levels, fatigue, nausea, headache, and swelling. If patients experience these side effects, or new or worsening side effects, they should talk with their doctor. A healthcare provider may recommend dose adjustments, or stopping or pausing treatment.
Weight gain is not a known side effect of Isturisa, but it is among the known symptoms of Cushing’s disease. Some evidence from clinical trials indicate that Isturisa is associated with reductions in body weight. Patients who gain weight while using Isturisa or experience other unexpected side effects should discuss them with their healthcare team.
Related Articles

 Fact-checked by
Fact-checked by