Recorlev (levoketoconazole) for Cushing’s disease
What is Recorlev for Cushing’s disease?
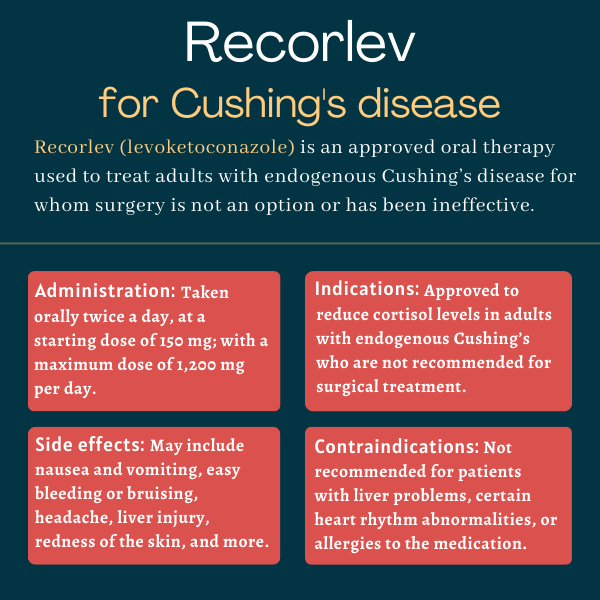
Recorlev (levoketoconazole) is an oral therapy approved to reduce higher than normal cortisol levels in adults with endogenous Cushing’s syndrome, including Cushing’s disease, for whom surgery is not an option or has been ineffective.
The therapy was originally developed by Strongbridge Biopharma, which was acquired by Xeris Pharmaceuticals in 2021.
Therapy Snapshot
| Brand Name: | Recorlev |
| Chemical Name: | Levoketoconazole |
| Usage: | Used to lower excessive cortisol levels in adults with endogenous Cushing’s syndrome for whom surgery is not an option or has been ineffective |
| Administration: | Oral tablets |
How does Recorlev work?
Endogenous Cushing’s is a form of the rare disease in which the body produces too much of a hormone called cortisol. Cortisol is a glucocorticoid — a steroid hormone produced by the adrenal glands that sit atop the kidneys — that is involved in several bodily processes. Among them are regulating the body’s stress response, controlling blood pressure, regulating blood sugar levels, and reducing inflammation.
Excess cortisol throws the body off balance, leading to Cushing’s wide range of symptoms. This can include weight gain or fat accumulation in specific body parts, fragile skin and pink or purple stretch marks, and high blood pressure and high blood sugar levels.
Endogenous Cushing’s is most commonly caused by a tumor in the brain’s pituitary gland — a form of the disorder called Cushing’s disease — but disease-causing tumors also may develop in other tissues and organs. In all cases, these tumors ultimately send signals that prompt the adrenal glands to produce excessive amounts of cortisol.
As such, surgical removal of these tumors is typically the first line of treatment to normalize cortisol levels. However, in some patients, surgery may be ineffective at lowering cortisol levels or is not an option.
Recorlev is an oral therapy that works by suppressing a group of enzymes in the adrenal glands that are involved in the production of cortisol and testosterone, another steroid hormone. By blocking cortisol production, the therapy is expected to reduce cortisol levels in the body, thereby easing Cushing’s symptoms.
The active ingredient in Recorlev, levoketoconazole, is derived from ketoconazole — an oral therapy approved in Europe as Ketoconazole HRA to reduce cortisol levels in patients with endogenous Cushing’s. The therapy is used off-label in the U.S. for that indication.
Who can take Recorlev?
Recorlev was approved by the U.S. Food and Drug Administration in December 2021 to reduce cortisol levels in adults with endogenous Cushing’s syndrome for whom surgery is not an option or failed to lower cortisol levels.
Who should not take Recorlev?
Recorlev is not recommended for anyone with liver disease, signs of liver damage, prior history of liver injury due to ketoconazole or any similar antifungal therapy, recurrent gallstones, or liver cancer.
Patients with certain abnormalities in their heart rhythm, and anyone taking medications that cause such irregularities, also should avoid the therapy.
Recorlev also is not recommended for patients with a known allergy to the medication, any of its ingredients, or to ketoconazole.
In addition, Recorlev should not be taken in combination with medications that affect liver function, and those that are processed or transported in the body by the enzymes and molecules suppressed by Recorlev; this is due to a higher risk of adverse reactions from such medications. Patients should confirm with their healthcare provider that they are not receiving any of these types of drugs.
Recorlev is not indicated for use in treating fungal infections.
How is Recorlev administered?
Recorlev is available in 150 mg round, pink tablets.
The recommended starting dose is 150 mg, taken orally twice daily with or without food. That dose can be increased gradually every two to three weeks, based on efficacy and tolerability, in 150 mg increments, up to a maximum of 1,200 mg per day. The maximum dosage can be given as 600 mg twice daily.
After establishing the maintenance dosage of Recorlev, urine cortisol levels should be monitored at least every one to two months, or as indicated. If levels remain higher than normal with the maximum recommended dosage, treatment discontinuation should be considered and an alternative therapy sought.
If a planned dose is missed, patients should take the next dose at the regularly scheduled time.
Recorlev in clinical trials
Recorlev’s approval was mainly supported by data from two international Phase 3 clinical trials: SONICS (NCT01838551) and LOGICS (NCT03277690). The trials involved a total of 166 patients — 12 of whom participated in both studies.
SONICS trial
SONICS evaluated the safety and effectiveness of Recorlev in 94 adults with endogenous Cushing’s syndrome whose urinary cortisol levels were at least 1.5 times higher than normal. None of the participants were eligible for radiation therapy or surgery.
The first two weeks and up to nearly five months of treatment were meant to find each patient’s optimal dose. That dose was then given for about six months in the second, maintenance part of the study, without any dose increase allowed during that period. Following that, patients were evaluated for six additional months while on treatment in the trial’s third part. Overall, the maintenance treatment period with Recorlev totaled one year.
Top-line data showed 31% of patients saw their urinary cortisol levels drop to a normal range after six months of maintenance treatment with Recorlev, without any dose increments — meeting the trial’s main goal.
Recorlev also was able to lessen symptoms, ease depression, and improve patients’ quality of life, while helping to control blood sugar levels in a subgroup of patients with both Cushing’s and diabetes.
Up to 22 months of Recorlev treatment safely led to sustained reductions in cortisol levels and multiple cardiovascular risk markers, while easing disease signs and symptoms, reducing depression, and improving quality of life.
LOGICS trial
LOGICS enrolled 84 adults with endogenous Cushing’s who had previously participated in SONICS, or who had never been treated with Recorlev and whose urinary cortisol levels were 1.5 times or higher than normal.
A total of 79 participants received Recorlev in the dose-optimization phase, and 39 on a stable dose for at least four weeks were randomly assigned to either remain on the medication or switch to a placebo for two months. This design allowed researchers to assess the effects of treatment withdrawal.
Top-line results showed that nearly all patients (95.5%) who switched to a placebo had increased urine free cortisol levels higher than 1.5 times the upper normal value. That compared with less than half (40.9%) of those who remained on Recorlev. Consistently, normal cortisol levels were observed in a greater proportion of patients who were always on Recorlev than among those who moved to a placebo (50% vs. 4.5%).
Continuous treatment with Recorlev also was associated with better outcomes, though the difference relative to the placebo group failed to reach statistical significance. Also, patients who switched to the placebo lost Recorlev’s cholesterol-lowering benefits.
After completing the placebo-controlled withdrawal phase, all participants were treated with Recorlev for another two months. By the end of that period, more than half (58%) had cortisol levels in the normal range, including 52% of those always on Recorlev and 64% of those who had switched to a placebo in the previous phase.
OPTICS trial
Patients who completed SONICS, LOGICS, or both trials were given the option to enroll in an open-label extension study called OPTICS (NCT03621280). A total of 51 people took part, all receiving Recorlev for up to three years. Long-term safety data from the trial also supported the therapy’s approval.
Common side effects of Recorlev
The most common side effects of Recorlev include:
- nausea and vomiting
- abnormally low blood potassium levels
- easy bleeding/easy bruising
- high blood pressure
- headache
- liver injury
- menstrual cycle irregularities
- skin redness
- fatigue
- abdominal pain or upset stomach
- joint inflammation and/or pain
- upper respiratory infection
- muscle pain
- heart rhythm abnormalities
- back pain
- insomnia or sleep disturbances
- swelling of the lower legs or hands.
Liver damage
There have been reports of serious liver injury in patients on Recorlev, regardless of treatment dosage. Also, cases of such injury resulting in death or requiring a liver transplant were reported in patients taking oral ketoconazole. As such, Recorlev is not recommended for patients with certain liver conditions, including cirrhosis, acute liver disease, or poorly controlled chronic liver disease, or a history of liver damage related to the use of ketoconazole or any similar antifungal therapy.
Markers of liver health, such as liver enzymes, should be monitored before starting the medication, and regularly during treatment, especially when increasing the dosage.
Recorlev should be immediately stopped if clear signs of liver damage are observed. Milder signs may prompt temporary discontinuation or dose modification.
Patients on Recorlev also should avoid excessive alcohol consumption.
Anyone experiencing pain on the upper right side of the stomach combined with nausea, unusual fatigue, a yellowish color on the skin or in the whites of eyes, or unusual bruising or bleeding while on Recorlev should immediately contact their healthcare provider.
Heart rhythm abnormalities
Recorlev may cause abnormalities in a person’s heart rhythm that can result in life-threating heart conditions. As such, the therapy is not recommended for patients with certain heart rhythm irregularities and for those taking medications that cause such abnormalities.
Patients starting on Recorlev should have their heart activity closely monitored before and during treatment. Given that lower than normal blood levels of potassium and/or magnesium can increase the risk of heartbeat irregularities, these should be corrected before patients start taking Recorlev, and then periodically monitored during treatment.
Caution is recommended when starting the therapy in patients with other risk factors for heart rhythm abnormalities such as heart failure or an abnormally slow and irregular heartbeat. Heart health monitoring should be more frequent in these patients.
If considerable signs of heartbeat abnormalities are detected, temporary or permanent discontinuation of Recorlev should be considered.
Patients should immediately call their healthcare provider if they experience severe lightheadedness or fainting while on Recorlev.
Hypocortisolism
Because it works by reducing cortisol production, Recorlev can cause hypocortisolism, or lower than normal levels of cortisol. This has the potential to lead to a life-threatening insufficiency of the cortisol-producing adrenal glands.
For this reason, patients should have their urine and blood cortisol levels closely examined, and be monitored for symptoms of hypocortisolism or adrenal insufficiency, during treatment with Recorlev. If these complications arise, healthcare providers should consider reducing the dose or discontinuing treatment altogether.
Patients experiencing symptoms of reduced adrenal function — such as nausea or vomiting, unusual fatigue, unexplained stomach pain, low blood pressure, loss of appetite, body aches, or dizziness — should contact their healthcare provider right away.
Allergic reactions
Allergic reactions have been reported in patients given Recorlev or ketoconazole. Recorlev should never be given to anyone with a known allergy to its ingredients or to ketoconazole. If an allergic reaction occurs, Recorlev should be stopped immediately.
Risks related to decreased testosterone
Recorlev may cause a reduction in blood testosterone levels, both in men and in women. In men, reductions in testosterone levels may cause symptoms such as breast enlargement, erectile dysfunction, and low sperm count, while in women it can lead to reduced libido and mood changes. If these symptoms occur, patients should inform their healthcare provider.
The therapy also may cause fertility problems.
Use in pregnancy and breastfeeding
Recorlev has not been thoroughly studied in women who are pregnant. However, findings from animal models suggest ketoconazole, a similar medication, may cause harm to a developing fetus, increase the risk of miscarriage, and lead to a difficult labor. Patients who are or plan to become pregnant should discuss this topic with their healthcare team and carefully weigh the potential benefits and risks of using Recorlev in these circumstances.
It remains unknown if Recorlev can pass into breast milk, and whether it can have any harmful effects on breastfed infants or on milk production in nursing patients. While low levels of ketoconazole have been detected in the breast milk of breastfeeding women, there are limited data on its effects. Due to the therapy’s potential risks to the breastfed infant, including liver toxicity, breastfeeding should be avoided during treatment with Recorlev and for one day after the final dose.
Cushing’s Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Targeted radiation therapy offers hope for tough Cushing’s cases
- Bone problems common in Cushing’s, but care varies across Europe: Study
- How Cushing’s disease has made me a better parent
- Blood thinner rivaroxaban prevents clots in ACTH-dependent Cushing’s
- Surgery offers best cortisol control for adrenal Cushing’s syndrome
- Turning negatives into positives keeps me out of the ‘why me’ pit
- Common Cushing’s test may miss aggressive tumors in some patients
- Weak bones, fractures prevalent in Cushing’s syndrome: Analysis
- We’re preparing to finally bring our newborn daughter home
- Surgery brings Cushing’s remission to 60% of patients over 20 years: Study
FAQs about Recorlev
Recorlev was approved by the U.S. Food and Drug Administration (FDA) in 2021 to reduce higher than normal cortisol levels in adults with endogenous Cushing’s syndrome. The FDA approval also indicates the treatment’s use for adults with Cushing’s disease, and for those for whom surgery is not an option or has been ineffective.
The potential interaction between Recorlev and alcohol has not been thoroughly investigated. However, given its potential to cause liver injury, Recorlev’s U.S. label recommends that patients starting treatment avoid drinking alcohol in excess, as it may increase the risk of serious side effects.
In the SONICS trial that supported the therapy’s approval, urinary cortisol levels dropped to normal levels in about two-thirds of analyzed patients (67%) by the fifth month after starting Recorlev treatment, which lasted 2-21 weeks. Reductions in certain symptoms also were reported within a time frame of just a few weeks to 5-6 months.
Recorlev may cause several side effects, most commonly nausea and vomiting, easy bleeding or bruising, headache, liver injury, redness of the skin, fatigue, and upset stomach.
Weight gain has not been reported as a side effect of Recorlev. In fact, treatment with Recorlev has been shown to lead to significant weight loss in clinical trials. Patients should talk with their healthcare team if they experience any unanticipated side effects of treatment.
Related Articles
 Fact-checked by
Fact-checked by