Signifor (pasireotide) for Cushing’s disease
What is Signifor for Cushing’s disease?
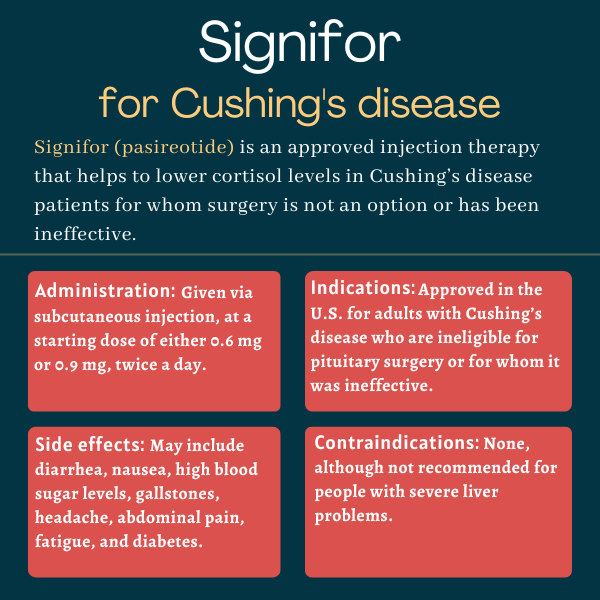
Signifor (pasireotide) is an injection therapy approved for adults with Cushing’s disease for whom pituitary surgery isn’t an option or has been ineffective.
Injected subcutaneously, or under the skin, it’s designed to lower cortisol levels and ease disease symptoms.
The medication was originally developed by Novartis, but its rights were acquired in 2019 by Recordati, which markets the therapy in the U.S. through its subsidiary Recordati Rare Diseases.
Therapy Snapshot
| Brand Name: | Signifor |
| Chemical Name: | Pasireotide |
| Usage: | Used to treat Cushing’s patients who are ineligible for or have failed surgery; can lower cortisol levels and ease disease symptoms |
| Administration: | Subcutaneous injection |
How does Signifor work?
Cushing’s disease is a form of Cushing’s syndrome wherein its hallmark excess levels of the hormone cortisol are caused by a tumor in the pituitary gland at the base of the brain.
The tumor makes the pituitary gland release excessive amounts of adrenocorticotropic hormone (ACTH), which stimulates the adrenal glands atop the kidneys to produce too much cortisol. Given that cortisol is involved in a number of bodily processes, excess levels of this hormone lead to a number of hormonal, physical, and psychological symptoms.
Surgically removing the pituitary tumor is the first line of treatment to normalize cortisol levels with Cushing’s disease. Some patients are ineligible for the procedure, however, and it can be ineffective in others. In such cases, medications to reduce cortisol can alleviate symptoms.
Signifor’s active ingredient, pasireotide, mimics the activity of somatostatin, a hormone that regulates several bodily functions by suppressing the release of other hormones, including ACTH. Importantly, the therapy targets four of five somatostatin receptor proteins, especially receptor 5, the most commonly found in Cushing’s disease tumors.
By binding to and activating key somatostatin receptor proteins in the pituitary gland, Signifor should lower ACTH production, reducing cortisol levels, and easing Cushing’s symptoms.
Who can take Signifor?
Signifor was approved by the U.S. Food and Drug Administration (FDA) in 2012 for treating adults with Cushing’s disease for whom pituitary surgery isn’t an option or has failed to sustainably reduce cortisol levels.
The decision made Signifor the first disease-modifying therapy approved for Cushing’s disease. The therapy also became the first and only subcutaneous, pituitary-targeted medication clinically proven to treat the disease.
In Europe, Signifor also was approved for the same indication in 2012. It’s approved in several other countries, including Canada and Australia.
Who should not take Signifor?
The prescribing information for Signifor lists no contraindications. It should be avoided in those with severe liver problems, however.
Signifor also should be used with caution by people with risk factors for QTc prolongation — a medical term that describes an extension of the interval between the heart contracting and relaxing — as it has been associated with cardiac arrhythmias.
How is Signifor administered?
Signifor is available as a single-dose glass ampule containing a clear and colorless solution. It comes in three different dose strengths: 0.3 mg/mL, 0.6 mg/mL, and 0.9 mg/mL.
The recommended starting dose is either 0.6 mg or 0.9 mg, administered by subcutaneous injection twice a day. Dosage can be reduced to 0.3 mg twice daily or increased up to 0.9 mg twice a day based on tolerability and clinical response, including changes in urinary cortisol levels. Dose reductions should be done in 0.3 mg decrements per injection.
People with moderate liver problems should start Signifor at 0.3 mg twice daily, with a maximum dose of 0.6 mg twice a day.
Before starting Signifor, patients should undergo blood tests to measure fasting blood sugar levels, along with potassium and magnesium levels. Liver tests, a gallbladder ultrasound, and a heart function test that looks for abnormalities should also be conducted before starting treatment. Patients with poorly controlled diabetes should have their anti-diabetic treatment regimen heavily optimized before starting Signifor.
It’s recommended that Signifor be injected into the thigh or abdomen. It can be self-administered at home by patients or caregivers who’ve been trained by a healthcare professional in how to prepare and perform injections. The injection site should alternate from dose to dose and injections shouldn’t be administered into areas that show signs of inflammation or irritation.
If a planned dose is missed, patients should take the next dose at the regular scheduled time.
Signifor in clinical trials
Signifor approvals were mainly supported by data from a Novartis-sponsored Phase 3 clinical trial called PASPORT-CUSHINGS (NCT00434148).
PASPORT-CUSHINGS trial
The trial evaluated the safety and effectiveness of two doses (0.6 and 0.9 mg) in 162 adults with Cushing’s disease whose urinary cortisol levels were at least 1.5 times higher than normal. Patients were recruited at more than 60 sites across North and South America, Europe, and Asia.
Most had persistent or recurrent Cushing’s despite pituitary surgery, while some had newly diagnosed disease and were not considered surgery candidates.
Participants were randomly assigned to receive one of the two doses, twice daily, for three months. After that, the dosage was maintained or increased based on the clinical response for another three months.
Following the completion of the six-month treatment period, patients entered the study’s six-month open-label phase, wherein all knew the dose they were receiving. Dose adjustments could be done at any time based on the clinical response.
The trial’s main goal was to assess the proportion of patients who saw their urinary cortisol levels return to normal after six months of treatment without requiring any dose increments.
Both doses of Signifor led to a reduction in urinary cortisol levels as early as one month after treatment initiation, results showed. At six months, 15% of those given the 0.6 mg dose and 26% of those on the 0.9 mg dose showed normalized cortisol levels.
Similar rates were observed after one year of treatment, with 13% of patients in the lower-dose group and 25% in the higher-dose group displaying normal cortisol levels. More than half (55%) of patients with normalized cortisol levels at six months continued to have them at one year.
More than 10% of patients in both groups achieved partial treatment responses at six months. These patients still had higher than normal cortisol levels, but showed a reduction of 50% or more from the start of the study.
In blood samples, the levels of cortisol and ACTH in circulation were also significantly lowered with treatment after six months and continued to decrease up to one year.
Signifor also lowered Cushing’s signs and symptoms after six and 12 months, including reductions in blood pressure, blood levels of fatty molecules, and body weight, as well as improvements in health-related quality of life. In patients with evaluable photographs, facial redness and fat deposits were also reduced.
In addition, in patients with a measurable pituitary tumor on MRI, treatment with the higher dose was associated with a mean reduction of 43.8% in tumor volume after a year.
Open-label extension
After a year of treatment, participants seeing benefits with Signifor could enter an open-label extension wherein all received the therapy for up to about six years.
Results from this part of the trial showed the observed reductions in urinary cortisol levels, as well as in blood levels of cortisol and ACTH, at one year were generally sustained after two and five years of treatment.
Long-term treatment with Signifor also resulted in sustained reductions in blood pressure and weight. Most patients saw other symptoms stabilize or diminish, including facial redness, pink or purple stretch marks, bruising, and fat pads.
Notably, given that there were different rates of symptom reductions, there was no placebo group, and study participants were allowed to take medications to reduce blood pressure, it’s unclear if these changes were caused by Signifor.
Ongoing trials
In 2013, a global, real-world study (NCT02310269) was launched to evaluate the three-year safety and effectiveness of Signifor when given alone or with other treatments in up to 200 adults with Cushing’s disease for whom surgery had failed or wasn’t an option.
Interim data showed that half the participants who started Signifor for the first time during the study saw their urinary cortisol levels normalize within the first month of treatment and this was maintained for at least nine months. Rates of cortisol control among those already being treated with Signifor remained generally stable over two years of treatment.
Common side effects of Signifor
The most common side effects of Signifor in clinical trials include:
- diarrhea
- nausea
- high blood sugar
- gallstones
- headache
- abdominal pain
- fatigue
- diabetes.
Hypocortisolism
Because it works by lowering ACTH production, Signifor can cause a reduction in blood cortisol levels and potentially result in hypocortisolism, or lower than normal cortisol levels.
Patients should be monitored for signs and symptoms of hypocortisolism, such as weakness, fatigue, loss of appetite, nausea, vomiting, low blood pressure, lower than normal blood sodium levels, and low blood sugar. If these occur, patients should immediately contact their healthcare provider, who should consider reducing the dose or discontinuing Signifor treatment and administer temporary cortisol replacement therapy.
High blood sugar and diabetes
Signifor may cause blood sugar levels to rise above normal — hyperglycemia, a hallmark symptom of diabetes. In clinical trials, most patients showed an increase in blood sugar levels in the first two weeks of treatment and some developed diabetes and pre-diabetes, a condition wherein blood sugar levels are higher than normal, but not as high as those normally associated with diabetes.
Patients starting Signifor should have their blood sugar levels measured before treatment and regularly thereafter. Such assessments should also be performed after any dose increase.
Patients with poor blood sugar control may be at a higher risk of hyperglycemia and associated complications with Signifor. Anti-diabetic therapy should be optimized for those with uncontrolled diabetes prior to initiating Signifor.
For patients developing hyperglycemia while on Signifor, medication to control diabetes should be initiated or adjusted according to standard of care. If this is ineffective, dose reduction or permanently discontinuing Signifor should be considered, while closely monitoring blood sugar levels.
Patients starting on an anti-diabetic medication due to treatment with Signifor should be closely monitored after Signifor is discontinued, especially if the anti-diabetic therapy has a risk of causing low blood sugar levels.
Heart rhythm abnormalities
Signifor may cause heart rhythm abnormalities, including bradycardia (slow heartbeat) and QTc prolongation (a longer interval between heart contraction and relaxion), which in some cases can result in weakness, dizziness, and fainting. Those starting Signifor should have their heart activity closely monitored before and during treatment.
Because lower than normal blood levels of potassium and/or magnesium can increase the risk of heartbeat irregularities, these should be corrected before starting Signifor and monitored periodically thereafter.
Caution is also recommended when starting Signifor in patients with heart conditions, those at higher risk for heart rhythm irregularities, and those taking medications that cause such abnormalities. These patients should undergo more frequent heart health monitoring.
Patients having severe lightheadedness or fainting with Signifor should immediately call their healthcare provider.
Liver injury
Increases in the levels of liver enzymes, suggestive of liver damage, have been reported in some patients taking Signifor. Therefore, markers of liver health should be monitored before starting treatment, and regularly thereafter.
In the presence of liver enzyme elevations, confirmed with repeated testing, Signifor treatment should be interrupted and the cause of these abnormalities should be investigated. If another likely cause is identified and levels return to normal or near normal in subsequent measurements, physicians may consider resuming Signifor with caution and close monitoring.
Gallstones
Patients on Signifor may develop gallstones and have associated complications, including inflammation and infection of the gallbladder and bile ducts, which carry bile from the liver to the gallbladder and intestines. These complications may be serious and require gallbladder removal surgery.
For this reason, patients should undergo ultrasonic examination of the gallbladder before and periodically during treatment with Signifor. If there is a suspicion of gallstones, patients should stop Signifor treatment and receive appropriate medication.
Patients having signs of gallstones, such as sudden pain in the upper right abdomen, yellowing of the skin and eyes, nausea, sudden pain in the right shoulder or between the shoulder blades, and fever with chills should inform their healthcare provider.
Pituitary hormone deficiency
Because Signifor mimics the effects of somatostatin, patients on the therapy may see reductions in the levels of pituitary hormones other than ACTH. Pituitary gland function should be monitored before initiating Signifor and during treatment, as clinically indicated.
Patients with a history of pituitary surgery and radiation therapy are at a higher risk of pituitary hormone deficiency.
Use in pregnancy and breastfeeding
Signifor has not been thoroughly studied in women who are pregnant or breastfeeding. However, based on animal studies, it may cause harm to the developing fetus and may be present in breast milk.
Patients who are pregnant or nursing, or plan to become pregnant or breastfeed, should discuss this with their healthcare team and carefully weigh the potential benefits and risks of using Signifor in these circumstances.
Signifor-associated reduction or normalization of blood cortisol levels may improve fertility in premenopausal women with Cushing’s disease.
Cushing’s Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- How I keep my body from overheating during the summer
- Korlym lowers blood sugar, weight in people with Cushing’s, diabetes
- These home modifications will help me live better with Cushing’s
- 1st Cushing’s patient dosed in ST-002 Phase 2 clinical trial
- Obesity screening in Cushing’s may aid bariatric surgery outcomes
- Ketoconazole with octreotide may be effective Cushing’s treatment
- IVF is proving challenging, so I lean on some helpful tips
- Pituitary surgery can increase risk of blood clots forming in veins
- Low-dose aspirin may be better at preventing thromboses in Cushing’s
- Happy Pride: A look into my illness and gender expression
FAQs about Signifor
The U.S. Food and Drug Administration (FDA) approved Signifor in December 2012 for adults with Cushing’s disease who aren’t eligible for pituitary surgery or for whom the procedure was ineffective. This made Signifor the first disease-modifying therapy approved for the condition.
The potential interaction between Signifor and alcohol has not been thoroughly investigated. Increases in liver enzymes, suggesting liver damage, have been reported in some patients taking Signifor, however. Because excessive alcohol consumption also can damage the liver, patients should discuss with their healthcare provider if it’s safe to drink while on the medication.
In the PASPORT-CUSHINGS trial that supported Signifor’s approval, reductions in urinary cortisol levels and Cushing’s signs and symptoms were observed as early as one month after starting treatment. Normalized urinary cortisol levels were observed as early as three months. Because each person is unique and can respond differently to a medication, patients are advised to talk with their healthcare team about how the therapy can help in their particular case.
The most commonly reported side effects of Signifor include diarrhea, nausea, high blood sugar, gallstones, headache, abdominal pain, fatigue, and diabetes. If patients have new or worsening side effects, they should discuss the issue with their doctor, who may recommend reducing their dosage.
Weight gain hasn’t been reported as a side effect of Signifor, but it’s a known symptom of Cushing’s disease. Clinical trial data suggest the therapy is associated with weight loss. Patients should talk with their healthcare team if they experience weight gain or any other unanticipated effects of treatment.
Related Articles

 Fact-checked by
Fact-checked by