FAQs about Ketoconazole
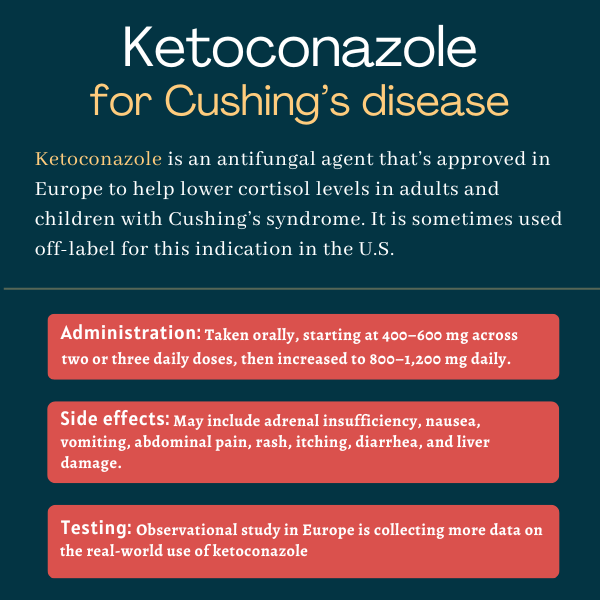
Ketoconazole is not approved by the U.S. Food and Drug Administration for Cushing’s disease, and it’s not known if or when the regulatory agency may approve the medication for this indication. In Europe, the therapy is approved for Cushing’s disease and other forms of endogenous Cushing’s syndrome in adults and children, 12 and older. In the U.S., it’s sometimes used off-label for that purpose.
Cushing’s disease symptoms are caused by the excessive levels of a hormone called cortisol. Ketoconazole can block the production of cortisol, thereby lowering its levels and helping to ease symptoms.
It’s recommended that people taking ketoconazole abstain from drinking alcohol as combining the two has reportedly led to patients experiencing flushing, rash, swelling, nausea, and headache.
Studies evaluating the effects of ketoconazole on Cushing’s patients vary widely in terms of treatment duration and dosing regimens. Data from five studies involving more than 250 patients showed that at a median follow-up of 7.5 months, a median 50% of the patients saw their cortisol levels normalize, meaning that some individuals may see the results of treatment within a few months. Cortisol normalization was most frequently seen when ketoconazole was administered at a dose between 600 and 800 mg per day.
The most common side effects of ketoconazole include adrenal insufficiency, rash, itching, liver damage, and digestive problems such as nausea, vomiting, abdominal pain, and diarrhea. Patients should discuss any unexpected effects of treatment with their healthcare team.
Related Articles
 Fact-checked by
Fact-checked by